Smoking and Heart Failure
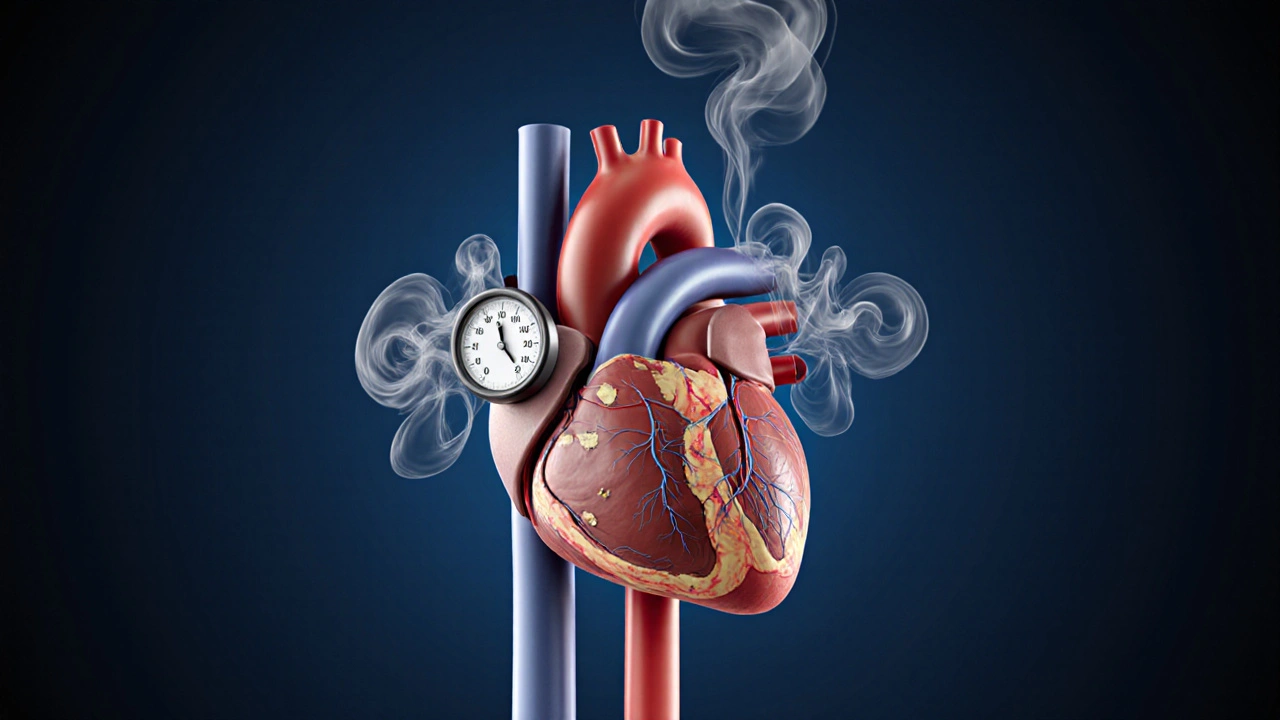
When dealing with smoking and heart failure, the combined impact of tobacco use on a failing heart, also known as tobacco use with cardiac insufficiency, you quickly see why the two are often mentioned together. Smoking, the inhalation of tobacco smoke that delivers nicotine and many harmful chemicals triggers inflammation, raises blood pressure, and reduces oxygen delivery. At the same time, heart failure, a condition where the heart cannot pump enough blood to meet the body’s needs makes the heart vulnerable to any extra stress. The link is clear: nicotine spikes heart rate, blood pressure, and sympathetic tone, which directly exacerbates heart failure symptoms. In practical terms, a smoker with heart failure often experiences more shortness of breath, faster fatigue, and a higher chance of hospital readmission. By understanding that smoking ⟶ worsens ⟶ heart failure, you can see why quitting is a top priority in any treatment plan.
Key Factors Linking Smoking to Heart Failure
First, nicotine, the primary addictive compound in tobacco stimulates the adrenal glands, raising catecholamine levels that make the heart work harder. Second, the carbon monoxide in smoke binds to hemoglobin, lowering oxygen transport and forcing the heart to pump more blood to deliver the same amount of oxygen—another strain on an already weak organ. Third, smoking accelerates cardiovascular disease, a group of disorders affecting the heart and blood vessels by promoting atherosclerosis, which narrows coronary arteries and reduces blood flow. These three mechanisms create a feedback loop: as the heart’s function declines, patients become less able to tolerate the physiological stress from nicotine and other smoke toxins, leading to more frequent exacerbations. Lifestyle changes—especially quitting smoking—can break this cycle. Studies show that quitting reduces mortality risk in heart failure patients by about 30% within five years, and it improves response to medications like beta‑blockers and ACE inhibitors.
Beyond the direct physiological impact, smoking habits intersect with other risk factors common in heart failure patients, such as hypertension, diabetes, and poor diet. Addressing the habit often opens the door to broader health improvements: better blood pressure control, weight loss, and increased exercise tolerance. Many clinicians recommend a step‑wise approach—counseling, nicotine replacement, and behavioral support—to maximize quit rates. When the quit attempt succeeds, patients typically notice less wheezing, improved energy, and a slower progression of heart failure. Below you’ll find a curated set of articles that dive deeper into these topics, from the chemistry of nicotine to practical tips for quitting, medication interactions, and the latest research on managing heart failure in smokers. Explore the collection to get the facts you need for better health decisions.
How Smoking Affects Congestive Heart Failure & How to Quit
Learn how smoking worsens congestive heart failure, the health benefits of quitting, and a step‑by‑step quit plan with medications, counseling, and cardiac rehab support.
Health and Wellness
How Smoking Affects Congestive Heart Failure and Proven Ways to Quit
Learn how smoking worsens congestive heart failure and follow a clear, heart‑friendly plan to quit. Get medical facts, quitting steps, and resources for lasting success.
Health and WellnessLatest Posts
Tags
- online pharmacy
- medication safety
- generic drugs
- medication
- dietary supplement
- side effects
- online pharmacy UK
- drug interactions
- mental health
- impact
- online pharmacies
- statin side effects
- dosage
- generic vs brand
- pediatric antibiotics
- antibiotic side effects
- skin health
- health
- pain relief
- dietary supplements




