CHF Smoking Risk Calculator
How Smoking Affects Your CHF Risk
This calculator estimates how smoking impacts your risk of complications if you have congestive heart failure. Enter your smoking history to see personalized risk insights.
Your Risk Assessment
Quick Takeaways
- Smoking speeds up the decline of heart function in people with congestive heart failure (CHF).
- Even a few cigarettes a day raise blood pressure and worsen fluid buildup.
- Quitting can improve exercise tolerance, reduce hospital visits, and add years to life.
- Combine medication, counseling, and a solid quit plan for the highest success rate.
- Support groups and mobile apps boost confidence during the toughest cravings.
What Is Congestive Heart Failure?
Congestive Heart Failure is a chronic condition where the heart cannot pump enough blood to meet the body’s needs, leading to fluid buildup in the lungs, legs, and abdomen. It affects about 6 million adults in the United States and 0.5% of Australians, with a median survival of three to five years after diagnosis if risk factors aren’t controlled. Symptoms include shortness of breath, swelling, fatigue, and a persistent cough. The disease is staged (A‑D) to guide treatment, from lifestyle tweaks (Stage A) to advanced therapies like ventricular assist devices (Stage D).
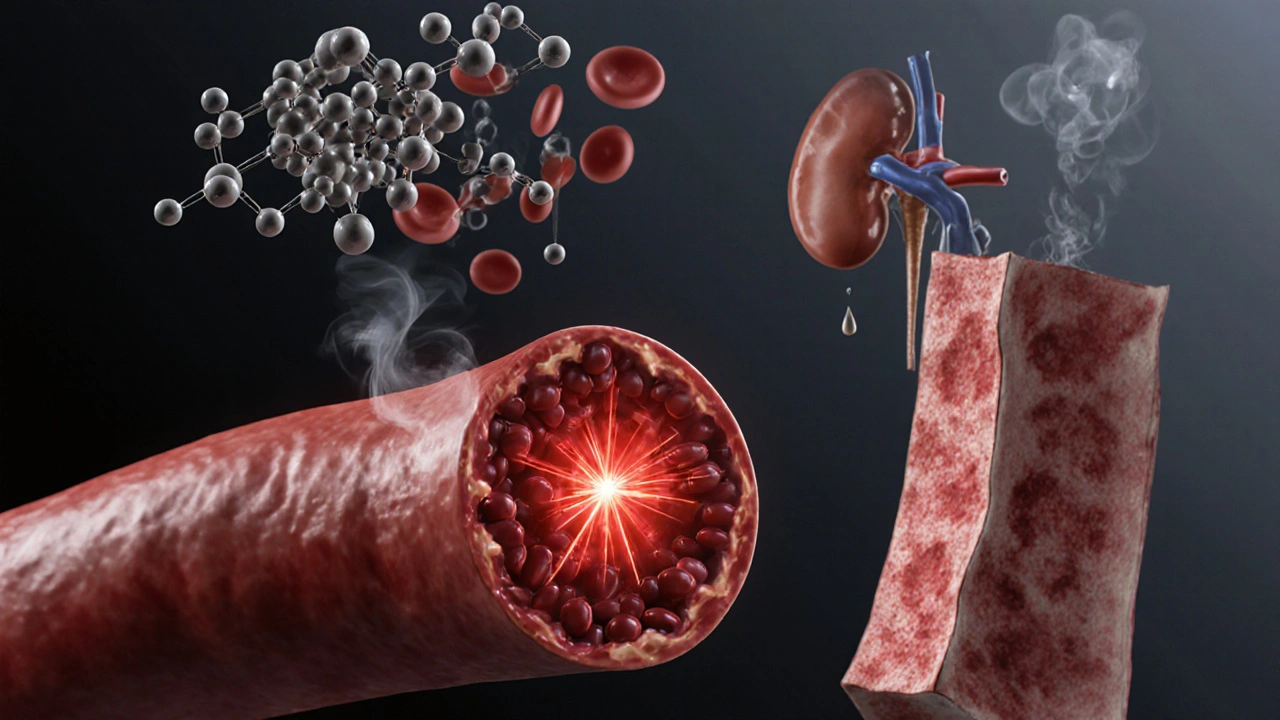
How Smoking Makes CHF Worse
Smoking isn’t just a habit; it’s a toxin bomb that hits the cardiovascular system from every angle. Here’s what happens when a smoker with CHF lights up:
- Blood pressure spikes. Nicotine causes a brief surge in adrenaline, tightening blood vessels and raising systolic pressure by 5‑10mmHg on average.
- Oxygen delivery drops. Carbon monoxide binds to hemoglobin 200 times more readily than oxygen, cutting the blood’s oxygen‑carrying capacity by up to 10% per pack‑day.
- Inflammation rises. Smoke particles trigger chronic inflammation, accelerating atherosclerosis and stiffening the heart muscle.
- Fluid retention worsens. Nicotine stimulates the renin‑angiotensin‑aldosterone system, prompting kidneys to retain sodium and water - the very problem CHF patients fight.
The combined effect is a faster decline in ejection fraction, more frequent dyspnea episodes, and a higher risk of hospitalization. Studies from the Australian Heart Foundation in 2023 showed smokers with CHF are 1.8times more likely to be readmitted within 30days compared to non‑smokers.
Measuring the Risk: Numbers That Matter
Putting the risk into numbers helps motivate change. In a 2022 cohort of 2,400 CHF patients:
- Current smokers (15% of the group) had an average ejection fraction of 31% versus 38% in never‑smokers.
- Each additional pack‑year added roughly 0.5% to the annual mortality risk.
- One‑year survival dropped from 82% in non‑smokers to 68% in smokers.
These figures illustrate why doctors flag smoking as a top modifiable risk factor alongside high blood pressure and uncontrolled diabetes.
Why Quitting Matters for Heart Failure Patients
Good news: the body starts repairing itself quickly after the last cigarette. Within 24hours, carbon monoxide levels normalize; after 2‑3 weeks, blood pressure and circulation improve; and after a year, the risk of coronary events drops to that of a non‑smoker.
For CHF patients specifically, quitting brings:
- Improved exercise capacity - up to a 15% increase in six‑minute walk distance.
- Reduced reliance on diuretics - studies show a 20% dose reduction after six months of abstinence.
- Fewer emergency visits - a 30% drop in heart‑failure‑related admissions, according to a 2024 Queensland health audit.
In short, quitting can add quality years and lessen the burden on caregivers.
Step‑by‑Step Plan to Quit Smoking
Quitting isn’t a one‑size‑fits‑all process, but the following roadmap covers the essentials for anyone battling both nicotine cravings and heart failure symptoms.
- Set a quit date. Choose a day within the next two weeks. Mark it on your calendar, tell family, and align it with a medical appointment if possible.
- Talk to your cardiologist. Ask about how your CHF meds (e.g., ACE inhibitors) might interact with nicotine‑replacement products.
- Pick a cessation method. Options include nicotine‑replacement therapy (NRT), prescription meds like varenicline, or behavioral counseling. See the comparison table below.
- Prepare your environment. Remove ashtrays, lighters, and any smoking triggers from home and car.
- Practice coping strategies. Deep‑breathing, short walks, or chewing sugar‑free gum can calm cravings without stressing the heart.
- Track progress. Use a journal or a free app to log smoke‑free days, cravings, and any side effects.
- Seek support. Join a local quit‑group, call a helpline, or ask a friend to be your “quit buddy.”
- Stay vigilant. If you feel shortness of breath or chest pain, contact your doctor immediately - it could be a heart‑failure flare‑up, not just nicotine withdrawal.
Choosing the Right Cessation Method
| Method | Typical Success Rate | Cost (AU$) | Heart‑Failure Considerations | Pros / Cons |
|---|---|---|---|---|
| Nicotine‑Replacement Therapy (patch, gum, lozenge) | 15‑25% | 30‑80 (monthly supply) | Low blood‑pressure impact; safe with ACE inhibitors | Easy to use; may cause skin irritation or throat soreness |
| Varenicline (Champix) | 30‑40% | 150‑250 (2‑month course) | Monitor for mood changes; no direct cardiac effect | Highly effective; possible nausea or vivid dreams |
| Bupropion (Zyban) | 20‑30% | 120‑200 (2‑month supply) | May raise blood pressure slightly; watch for seizure risk | Works for those who dislike nicotine; can aid depression |
| Behavioral Counseling (in‑person or telehealth) | 10‑20% | Free‑to‑low (public health services) | Focuses on stress management, key for CHF patients | Requires time commitment; best when combined with medication |
| E‑cigarettes (vaping) | 5‑10% | 50‑150 (device + e‑liquid) | Potential lung irritation; not recommended for CHF | Appealing flavor; health risks still uncertain |
Managing Cravings Without Overloading the Heart
Cravings peak between days 3‑7 and then fade. Use these heart‑friendly tactics:
- Hydration. Sip water every 15minutes; it reduces nicotine urge and helps renal function.
- Light activity. A 5‑minute walk at a comfortable pace improves circulation without stressing the heart.
- Deep‑breathing. Inhale for 4seconds, hold 2seconds, exhale for 6seconds. Repeat five times.
- Distraction kit. Keep sugar‑free gum, a stress ball, and a short‑story app handy.
If a craving feels overwhelming, use a short‑acting NRT product (gum or lozenge) while monitoring blood pressure - a quick check on a home monitor can reassure you.
Supporting Resources Tailored for CHF Patients
Finding the right help makes the difference between a short‑lived attempt and lasting change.
- Quitline Australia offers free 24/7 phone counseling and can coordinate with your cardiology team.
- Local hospitals in Sydney run “Heart Health & Smoke‑Free” workshops that blend cardiac rehab with quit‑support.
- Mobile apps like QuitBuddy and MyHeart have built‑in CHF symptom trackers to alert you if a craving episode coincides with worsening edema.
- Peer‑support groups (often hosted by the Heart Foundation) let you share stories with others who understand both heart failure and nicotine addiction.
Common Myths About Smoking and Heart Failure
Myth1: "A few cigarettes won’t hurt because my doctor gives me meds." Nope. Even low‑level smoking negates up to 50% of medication benefits.
Myth2: "Switching to vaping is safe for my heart.” The aerosol still contains nicotine and chemicals that can raise blood pressure.
Myth3: "I’m too old to quit.” Age only makes quitting more rewarding - older adults see a 40% drop in mortality when they stop.
Putting It All Together
Think of quitting as the most powerful medicine you can add to your CHF treatment plan. It works hand‑in‑hand with ACE inhibitors, beta‑blockers, and lifestyle advice. Start with a clear date, pick a method that fits your health profile, and lean on the resources listed above. Your heart will thank you with better stamina, fewer hospital trips, and a longer, fuller life.
Frequently Asked Questions
Can I use nicotine patches while taking my heart‑failure meds?
Yes. Nicotine patches deliver a steady low dose of nicotine that doesn’t spike blood pressure. Talk to your cardiologist to confirm the dose fits your current regimen, especially if you’re on ACE inhibitors or beta‑blockers.
How soon will I feel better after quitting?
Within two weeks you’ll notice less shortness of breath during daily tasks. By three months, exercise capacity often improves by 10‑15%, and fluid retention usually drops, allowing lower diuretic doses.
Is it safe to quit cold turkey with CHF?
Going cold turkey can trigger intense cravings and stress, which may raise heart rate and blood pressure. For most CHF patients, a gradual approach with NRT or medication under doctor supervision is safer and more successful.
Do e‑cigarettes help me quit?
Evidence shows e‑cigarettes have a low success rate (5‑10%) and still expose you to nicotine and other chemicals that can worsen blood pressure. Traditional FDA‑approved methods are recommended for CHF patients.
What if I slip and smoke a cigarette?
A slip isn’t a failure. Record the trigger, discuss it with your quit coach, and get back on track. One cigarette won’t erase weeks of progress, but recurring slips can signal the need for stronger support.







Fatima Sami
7 October 2025The calculator's interface could benefit from clearer labeling of the pack-year input field.
Arjun Santhosh
7 October 2025I tried the tool yesterday and kinda liked the vibe, but the drop‑down says "yes" or "no" without telling you what to pick – kinda confusing lol.
Also, the result area just shows blanks until you click, which makes me think the page is broken.
Overall, decent attempt, just needs a bit more polish.
Stephanie Jones
7 October 2025When I contemplate the silent dance between nicotine and a failing heart, I am reminded that each puff is a tiny rebellion against the body's desperate pleas.
The chemistry of smoking injects carbon monoxide, which masquerades as oxygen, stealing the precious lifeline that a compromised heart so desperately clings to.
In the realm of congestive heart failure, even a modest increase in vascular resistance can tip the scales toward fluid overload and breathlessness.
Research consistently shows that smokers with CHF have higher hospitalization rates, a fact that feels like a cruel punch to those already battling exhaustion.
Moreover, nicotine spikes adrenaline, accelerating heart rate and forcing an already overworked myocardium to pump harder, sooner.
This relentless pressure erodes the delicate balance of preload and afterload, leading to a cascade of worsening edema.
One could argue that the habit is not merely a personal choice but a hidden accomplice in the disease's progression.
The psychological grip of addiction, however, shrouds the path to quitting in foggy uncertainty.
Yet, each day without a cigarette is a small victory, a whispered promise to the heart that it might yet recover.
Studies highlight that cessation can improve ejection fraction within weeks, offering a glimmer of hope amidst the gloom.
The body, surprisingly resilient, begins to clear carbon monoxide, allowing oxygen transport to normalize.
Simultaneously, blood pressure drops, reducing the strain on the already weakened ventricular walls.
These physiological shifts translate into better exercise tolerance and fewer acute decompensations.
Thus, the decision to quit is not simply a lifestyle tweak; it is a therapeutic intervention with measurable outcomes.
In the end, the choice to extinguish the ember is a profound act of self‑compassion, gifting the heart a chance to beat a little longer.
Nathan Hamer
7 October 2025Wow, that was beautifully haunting, Stephanie! 🌟 Your words paint the struggle in vivid colors, and I totally agree-quitting isn’t just a habit change, it’s a life‑saving therapy! 🙌 Keep spreading the optimism, every little step counts.
Tom Smith
7 October 2025Ah, the classic ‘quit smoking, save your heart’ sermon-how original. If sarcasm were a medication, we’d all be cured by now. But seriously, kudos for the reminder; maybe the next time we’ll get a calculator that actually computes the *effort* required.
Kyah Chan
8 October 2025While the intent of the presented tool is commendable, its execution suffers from a paucity of user‑centric design principles; the absence of contextual tooltips and the ambiguous labeling of input fields detract from its efficacy. Additionally, the script lacks validation for non‑numeric entries, which could result in runtime exceptions. A thorough usability audit coupled with adherence to accessibility standards is advisable before deployment.