CHF Smoking Impact Calculator
Adjust the sliders to see how smoking affects your CHF risk and potential recovery benefits.
Key Takeaways
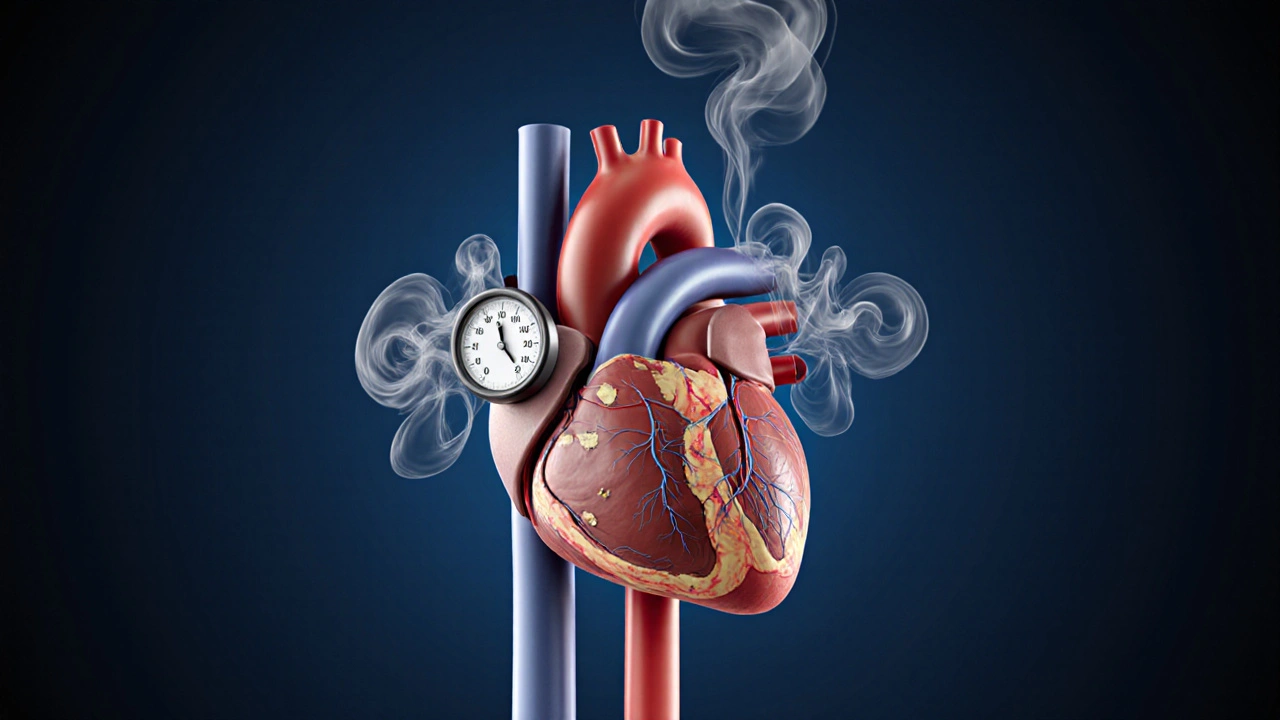
- Smoking speeds up the progression of congestive heart failure (CHF) by raising blood pressure, damaging blood vessels, and lowering oxygen delivery.
- Quitting smoking can lower hospital readmission rates for CHF patients by up to 30% within a year.
- Evidence‑based quit‑plans combine medication (NRT, bupropion, varenicline), counseling, and heart‑friendly lifestyle changes.
- Cardiac rehabilitation programs often integrate smoking‑cessation support tailored to CHF limitations.
- Resources from the American Heart Association and WHO provide free tools, phone lines, and online trackers.
Why Smoking Matters for Congestive Heart Failure
When it comes to heart health, Congestive Heart Failure is a condition where the heart can't pump enough blood to meet the body's needs. The heart muscle becomes weakened, fluid builds up in the lungs and legs, and everyday activities feel exhausting. Adding Smoking to the mix turns a tough situation into a medical emergency.
Every cigarette delivers nicotine, carbon monoxide, and thousands of toxins. These substances raise heart rate, constrict blood vessels, and increase the workload on an already strained heart. For a person with CHF, the extra demand can trigger:
- Higher blood pressure - the arteries become stiffer, forcing the left ventricle to push harder.
- Reduced oxygen transport - carbon monoxide binds to hemoglobin more tightly than oxygen, leaving tissues starved.
- Inflammation and plaque buildup - smoking accelerates atherosclerosis, narrowing coronary arteries and limiting blood flow to the heart muscle.
- Arrhythmias - nicotine spikes adrenaline, which can cause irregular heartbeats that are dangerous in CHF.
Data from the American Heart Association shows that smokers with CHF are 2-3 times more likely to be hospitalized for acute decompensation than non‑smokers. The World Health Organization estimates that tobacco‑related heart disease accounts for roughly 7 million deaths worldwide each year, a sizable share of which involve heart‑failure patients.
What Happens When You Quit?
Stopping smoking reverses many of the harmful mechanisms within weeks. Blood pressure often drops 5-10mmHg within the first month, and carbon monoxide levels return to normal within 24hours, improving oxygen delivery to tissues. Long‑term benefits include:
- 30-40% lower risk of CHF progression over five years.
- Reduced need for high‑dose diuretics, because fluid balance stabilizes.
- Improved exercise tolerance, which is key for cardiac rehab.
- Lower mortality: a 2023 cohort study of 1,200 CHF patients found a 22% drop in all‑cause death among those who quit within the first year.
In short, quit smoking isn’t just a lifestyle choice; it’s a clinical intervention that can shave months or even years off the disease trajectory.

Building a Quit Plan That Works With CHF
Many quit‑plans are one‑size‑fits‑all, but CHF patients need a strategy that respects limited stamina, medication interactions, and the risk of sudden blood‑pressure changes. Below is a step‑by‑step roadmap you can follow or share with your cardiology team.
- Get a medical clearance - Ask your cardiologist if any prescribed drugs (e.g., beta‑blockers) might affect nicotine‑replacement dosage.
- Set a quit date - Choose a day within the next two weeks. Mark it on your calendar and tell a trusted friend or family member.
- Choose a cessation aid - Options include Nicotine Replacement Therapy (NRT), bupropion, and varenicline. See the comparison table below for details.
- Enroll in counseling - Phone quit lines, online chat groups, or in‑person sessions at a cardiac rehab center add accountability.
- Monitor heart symptoms - Keep a log of any chest discomfort, palpitations, or sudden shortness of breath, and report changes to your doctor.
- Celebrate milestones - Reward yourself at 1week, 1month, and 3months with heart‑healthy treats (e.g., a fresh‑fruit smoothie).
Pharmacologic Aids: What Works Best for CHF Patients?
Below is a side‑by‑side look at the most common medicines and devices used to curb cravings. The data reflect studies up to 2024 and are vetted by cardiology societies.
| Aid | How It Works | Typical Dose for CHF | Key Pros | Potential Cardiac Concerns |
|---|---|---|---|---|
| Nicotine Replacement Therapy (NRT) | Delivers low‑level nicotine via patch, gum, lozenge, inhaler, or nasal spray. | Patch 21mg/24h for 6weeks, then taper. | Easy to use, no prescription needed, minimal impact on heart rate. | High doses may raise blood pressure; monitor if you have uncontrolled hypertension. |
| Bupropion | A non‑nicotine antidepressant that reduces cravings and withdrawal symptoms. | 150mg once daily for 3days, then 150mg twice daily for 7-12weeks. | Effective for people with depression; does not increase heart rate. | Can raise blood pressure in a small subset; avoid if you have seizure history. |
| Varenicline | Partial nicotine‑receptor agonist that blunts the rewarding effect of smoking. | 0.5mg daily for 3days, then 0.5mg twice daily for 4days, then 1mg twice daily for 11weeks. | Highest quit rates in meta‑analyses; works well for heavy smokers. | May cause mood changes; discuss with cardiologist if you have recent arrhythmias. |
Integrating Smoking Cessation Into Cardiac Rehabilitation
Cardiac rehab programs are not just about treadmill time; they’re a holistic platform where smoking cessation gets a seat at the table.
- **Education sessions** - Nurses explain how each puff adds extra workload to the failing heart.
- **Behavioral therapy** - Cognitive‑behavioral tools address stress triggers that often lead to a cigarette.
- **Medication coordination** - Rehab pharmacists adjust NRT or prescription meds to fit your heart‑failure regimen.
- **Exercise monitoring** - As you gain stamina, cravings often fade because nicotine’s stimulant effect becomes less needed.
Evidence from a 2022 multi‑center trial showed that CHF patients who attended a 12‑week rehab program with embedded cessation counseling were 45% more likely to stay smoke‑free at 12‑month follow‑up compared to those who only received standard care.

Practical Tips for Staying Smoke‑Free When You Have CHF
Even with the best plan, temptation can strike. Here are real‑world hacks that have helped patients keep the habit at bay:
- Carry a “stress‑relief kit” - Include sugar‑free gum, a small stress ball, and a list of heart‑friendly activities (short walk, breathing exercise).
- Swap rituals - If you smoked with coffee, switch to herbal tea or add a slice of lemon for a new flavor cue.
- Use a smartphone app - Apps that track cravings and reward days smoke‑free can sync with your smartwatch’s heart‑rate monitor, giving you instant feedback.
- Stay hydrated - Dehydration worsens CHF symptoms and can make cravings feel more intense.
- Lean on your care team - Schedule quick check‑ins with your nurse after any “trigger” event.
Resources and Support Networks
Finding the right help matters. Below are free, reputable sources you can tap into right now:
- American Heart Association Quitline - 1‑800‑A‑HEART (1‑800‑243‑2778). Offers personalized counseling and can connect you with local cardiac rehab centers.
- World Health Organization “Tobacco Free” portal - Provides multilingual guides, videos, and a global map of nearby support groups.
- CDC’s “Tips From Former Smokers” campaign - Short videos that feature real CHF patients sharing their quit stories.
- Local hospital cardiac rehab departments - Most have integrated smoking‑cessation modules; ask for a referral.
Next Steps: Putting It All Together
If you’ve read this far, you’re ready to take action. Here’s a quick checklist you can print out:
- Discuss your intention to quit with your cardiologist and get medication clearance.
- Pick a quit date within the next 14 days.
- Choose a cessation aid (NRT, bupropion, or varenicline) based on the comparison table.
- Enroll in a counseling program - phone line, online chat, or cardiac rehab.
- Track your heart symptoms daily for the first month and report any changes.
- Reward yourself at 1‑week, 1‑month, and 3‑month milestones with heart‑healthy treats.
Remember, quitting isn’t a sprint; it’s a marathon that your heart can finally run without the extra weight of tobacco.
Frequently Asked Questions
Will nicotine replacement therapy raise my blood pressure?
Low‑dose NRT (e.g., a 21mg patch) usually has a minimal impact on blood pressure, but it’s wise to monitor readings during the first two weeks, especially if you already have hypertension.
Can I use both bupropion and a nicotine patch?
Yes. Many clinicians prescribe a combination because the patch smooths cravings while bupropion tackles mood swings. Your doctor will adjust the doses to avoid overstimulation.
Is it safe to start varenicline if I’m on a beta‑blocker?
Generally, yes. Varenicline does not directly interact with beta‑blockers. However, because it can affect mood, schedule a brief check‑in with your cardiologist during the first weeks.
How quickly will my heart function improve after quitting?
Within 48hours, carbon monoxide levels normalize, improving oxygen delivery. Blood pressure often drops within 1-2weeks, and exercise tolerance typically rises noticeably after 4-6weeks of consistent abstinence.
What if I slip and smoke a cigarette?
Don’t view it as a failure. Record the trigger, discuss it with your counselor, and get back on track immediately. A single slip rarely reverses long‑term heart‑health gains if you resume quitting right away.






Ria M
7 October 2025In the grand theater of mortality, smoking is the villain that stalks the fragile heart, whispering false promises of solace while tightening its grip on the beleaguered myocardium. The soot of each inhalation settles like dust on the arches of our circulatory cathedrals, eroding the very foundations upon which life’s symphony is performed. In congestive heart failure, the heart is already a weary actor, its stage crowded with fluid, its lines faltering; add nicotine, and the script collapses into chaos.
One must recognize that the nicotine molecule is a tyrant, coercing the sympathetic nervous system into a relentless drumbeat, a metronome of hypertension that the failing heart cannot ignore. The carbon monoxide, that silent assassin, binds with hemoglobin, stealing oxygen from tissues that already gasp for breath, as if the audience were held hostage in a dimly lit auditorium.
Yet, hope is not a distant echo. The cessation of smoking is a rebellion, a coup d’état against the tyranny of addiction, and the heart, though battered, is resilient. Within days, arterial pressure may retreat, the blood’s viscosity thins, and the lingering clouds of carbon monoxide disperse like fog at sunrise. In weeks, the rhythmic cadence of the heart steadies, offering a reprieve to those mired in the tumult of CHF.
The data, though presented in sterile tables, sings a story of redemption: a 30‑40% reduction in disease progression, a tangible decline in hospital readmissions, a measurable improvement in quality of life. It is incumbent upon each patient to grasp this narrative and rewrite their own ending, to replace the ember of a cigarette with the flame of determination.
Thus, let the heart’s battered walls hear the clarion call: quit, and you shall not merely survive, but you shall begin to truly live, unshackled from the ash that once bound you.
Michelle Tran
7 October 2025🔥🚭 Love the motivation, totally gonna try quitting! 🙌
Caleb Ferguson
8 October 2025From a clinical standpoint, the interplay between nicotine-induced vasoconstriction and already compromised cardiac output is a key driver of exacerbations in CHF patients. Reducing nicotine exposure can lower systemic vascular resistance, easing the afterload on the failing heart. It also improves oxygen transport, which is vital for tissue perfusion. I’d recommend a coordinated plan involving your cardiology team, a smoking cessation specialist, and possibly a cardiac rehab program to maximize support.
Delilah Jones
8 October 2025Don’t underestimate the power of a firm quit date; it forces your mind to lock in the change. If you keep wavering, the heart will keep paying the price.
Pastor Ken Kook
8 October 2025Listen, buddy, every puff is like adding another weight plate on a barbell you can’t lift.
When you quit, you’ll notice the breath coming easier after a few days - that’s the CO clearing out.
Just keep your meds handy, and watch those blood‑pressure numbers drop like a stone in a pond.
Stay strong, you’ve got this! :)
Jennifer Harris
8 October 2025The subtle shift in arterial tone after cessation often goes unnoticed until we measure it, yet it signals a profound physiological reset. By tracking your daily blood pressure trends, you can visualize the benefit beyond the abstract advice. Maintaining a calm routine will also temper the stress response that sometimes fuels relapse.
Northern Lass
8 October 2025While the author’s earnest exhortation is commendable, one must question the underlying assumption that nicotine cessation alone suffices to arrest the inexorable decline of congestive heart failure. The intricate tapestry of cardiac pathology is woven from genetic predisposition, socioeconomic determinants, and environmental toxins beyond tobacco. Moreover, the reliance on pharmaceutical aids such as varenicline skirts the broader discourse on holistic, non‑pharmacological interventions. To attribute a singular agency to smoking neglects the multifactorial nature of cardiovascular demise. In summation, the narrative, though well‑intentioned, simplifies a labyrinthine clinical reality.
Johanna Sinisalo
8 October 2025As a supportive coach, I encourage you to view quitting as a series of attainable milestones rather than an all‑or‑nothing battle. Celebrate each smoke‑free day with a heart‑healthy reward, such as a fresh salad or a short stroll. Pair your cessation plan with the cardiac rehab exercises already prescribed; the synergy will amplify benefits. Remember, consistency builds confidence, and confidence fuels perseverance.
surender kumar
8 October 2025Ah, the moral crusade against a habit that menaves the soul while claiming health; such sanctimony is deliciously ironic. One would think a smoker could at least respect the fragile organ that keeps him alive, yet folly persists. Spare us the self‑righteous pamphlets and let actions speak louder than rhetoric.
Justin Ornellas
8 October 2025Permit me to correct a grammatical nuance: the phrase "quit smoking" functions as a gerund, not a noun, and thus should be treated accordingly in prose. Beyond semantics, the philosophical implication is clear: emancipation from nicotine is an act of self‑actualization, a Nietzschean overcoming of base impulses. Empirical evidence substantiates this claim, with measurable reductions in morbidity. The patient, therefore, must seize agency, lest the heart be surrendered to deterministic decay. In sum, the cessation path is both scientifically sound and existentially profound.