Bile acid diarrhea isn’t just another case of IBS. It’s a specific, treatable condition that affects up to 30% of people diagnosed with IBS-D-yet most never hear the name. If you’ve had chronic watery diarrhea for months or years, especially after meals or at night, and nothing seems to help, bile acid diarrhea could be the real culprit. Unlike IBS, which is often managed with broad lifestyle changes, bile acid diarrhea has clear causes, reliable tests, and targeted treatments. The good news? Once diagnosed, most people see major improvements in just a few days.
What Exactly Is Bile Acid Diarrhea?
Your liver makes bile to help digest fats. Normally, 95% of bile acids are reabsorbed in the last part of your small intestine, called the terminal ileum, and recycled back to the liver. In bile acid diarrhea (BAD), this system breaks down. Too much bile ends up in your colon, where it acts like a laxative-pulling water in, speeding up movement, and triggering urgent, watery stools. There are three types:- Type I: Caused by damage or removal of the ileum-think Crohn’s disease, surgery, or radiation.
- Type II: No obvious cause. This is the most common and often mistaken for IBS-D.
- Type III: Linked to other conditions like gallbladder removal, celiac disease, or chronic pancreatitis.
Research shows people with BAD have faster stool transit-around 18 hours versus 24 in healthy people. Their gut microbiome is also different, with less Bifidobacteria and more E. coli, which may worsen bile acid irritation.
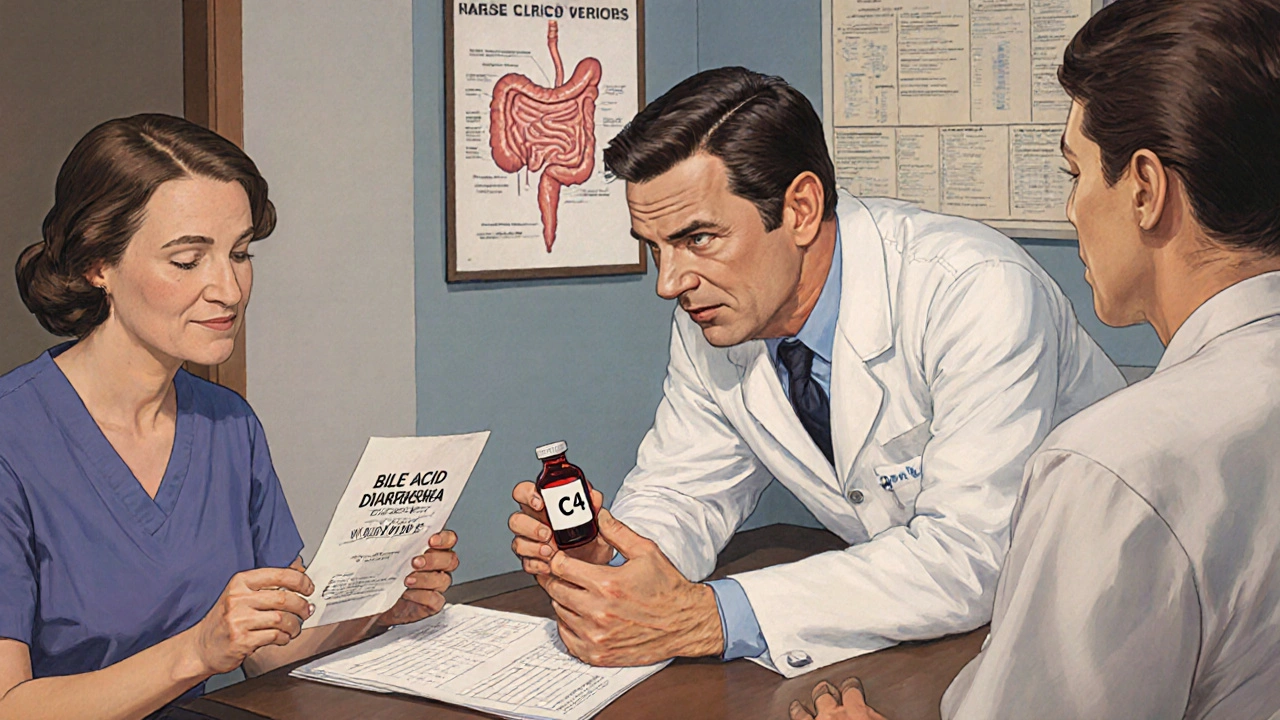
How Is It Diagnosed?
Most doctors don’t test for BAD unless you push for it. That’s why it takes an average of six years to get diagnosed. But there are reliable ways to confirm it.- SeHCAT test: The gold standard outside the U.S. You swallow a radioactive tracer that mimics bile acids. A scan after 7 days shows how much was reabsorbed. Below 15% retention means severe malabsorption. Problem? It’s not available in 90% of U.S. hospitals.
- Serum C4 test: Measures a bile acid precursor. Levels above 15.3 ng/mL suggest BAD. This blood test is becoming more common and is 77-78% accurate.
- FGF-19 test: Fibroblast growth factor 19 tells your liver to stop making bile. If levels are below 85 pg/mL, your body isn’t getting the signal to slow down production. This test is gaining traction in specialty clinics.
- Fecal bile acid test: Measures bile acids in a 48-hour stool sample. Highly accurate but requires special labs and strict collection.
Many doctors start with a trial of bile acid binders. If your diarrhea improves within 2-3 days, it’s likely BAD. No need to wait for expensive tests if symptoms respond.
Bile Acid Binders: The First-Line Treatment
These medications trap bile acids in your gut so they can’t reach the colon. Three are approved:- Cholestyramine (Questran): The oldest. 4 grams once or twice daily. Works well, but it’s chalky, gritty, and causes constipation in 20-30% of users. Many quit because of the taste.
- Colestipol (Colestid): Similar to cholestyramine but slightly less gritty. Dose: 5 grams once or twice daily.
- Colesevelam (Welchol): The most tolerable. Comes in tablets or powder. Dose: 1.875-3.75 grams daily. Only 5% report constipation. It’s also FDA-approved for cholesterol and type 2 diabetes, so it’s familiar to doctors.
Studies show about 70% of people with confirmed BAD respond to binders. Symptoms often improve within 48 hours. But adherence is a problem-35% stop within six months because of taste or side effects.
Pro tip: Mix cholestyramine or colestipol with water, apple juice, or applesauce. Don’t take it dry. Take it 1 hour before or 4 hours after other meds-it can interfere with absorption.
Dietary Changes That Actually Work
Medication helps, but diet is your daily shield. You don’t need to go gluten-free or keto. You need to control fat and fiber.- Keep fat low: Aim for 20-40 grams per day. Fat triggers bile release. Cutting fat below 30 grams daily reduces stool frequency by 40%. Avoid fried food, fatty meats, butter, cream, and full-fat dairy.
- Use soluble fiber: Psyllium husk (5-10 grams daily) binds bile acids and firms up stool. Take it 15-30 minutes before meals with a full glass of water. Studies show a 35% drop in daily bowel movements.
- Eat smaller, more frequent meals: Three big meals flood your system with bile. Five or six small meals spread the load. Cleveland Clinic data shows this cuts post-meal urgency by 25%.
- Avoid triggers: Caffeine (coffee, tea, soda) speeds up colon movement by 15-20%. Artificial sweeteners like sorbitol and xylitol pull water into the gut. Alcohol and spicy foods can worsen symptoms for some.
Some people find success with the Specific Carbohydrate Diet (SCD), which cuts out complex carbs. A 2019 survey found 45% of BAD patients improved on SCD. But it’s restrictive. Start simple: reduce fat, add psyllium, and track what triggers you.
Real Patient Experiences
On forums and support groups, common themes emerge:- “I thought I had IBS for 8 years. After starting colesevelam and cutting out fried chicken, my diarrhea dropped from 6 times a day to 1-2.”
- “Cholestyramine made me constipated. I cut the dose in half and added psyllium. Now I’m fine.”
- “I started taking psyllium before every meal. No more greasy, floating stools. That was my biggest clue.”
- “Colesevelam costs $400 a month without insurance. I switched to cholestyramine and found a discount pharmacy. It’s $60 now.”
Many report nocturnal diarrhea-52% have at least 3 night-time bathroom trips weekly. Fecal incontinence happens in 41% during flare-ups. But those who combine binders and diet see 68% symptom improvement.
What’s Next for BAD Treatment?
The future looks promising. Researchers are testing FGF19 analogs-drugs that mimic the body’s natural signal to stop bile production. A 2023 trial showed 72% symptom improvement in refractory cases. That’s bigger than any binder.Genetic testing is also emerging. Variants in genes like TGR5, FXR, and FGF19 may soon help identify who’s at risk before symptoms start.
Digital tools are helping too. Apps like BAD-Score use AI to predict flares based on diet, sleep, and stress. The BAD Tracker app lets users log meals, symptoms, and meds to spot patterns.
When to See a Specialist
If you’ve had chronic diarrhea for more than 4 weeks-especially if you’ve been diagnosed with IBS-D-ask your doctor about BAD. Don’t accept “it’s just IBS” as an answer. Request a serum C4 test or a trial of colesevelam. If your doctor isn’t familiar, ask for a referral to a gastroenterologist who specializes in functional bowel disorders.Many primary care providers still rely on outdated info. But places like Mayo Clinic now screen all IBS-D patients for BAD as part of their standard protocol. That’s led to a 35% drop in unnecessary colonoscopies.
Bottom Line
Bile acid diarrhea isn’t rare. It’s hidden. And it’s treatable. You don’t need to live with daily urgency, nighttime bathroom runs, or greasy stools. Start with a low-fat diet and psyllium. Talk to your doctor about a bile acid binder trial. Get a C4 blood test if possible. Most people get their life back in under a week.If you’ve tried everything for IBS and nothing stuck, it might not be IBS at all. It might be bile acid diarrhea.
Can bile acid diarrhea be cured?
Bile acid diarrhea isn’t usually “cured” unless the underlying cause is fixed-like healing Crohn’s disease or replacing a resected ileum. But for most people, especially Type II (idiopathic), it’s managed very well with binders and diet. Symptoms can disappear completely with the right treatment plan.
Is bile acid diarrhea the same as IBS-D?
No. IBS-D is a diagnosis of exclusion-meaning doctors rule out other causes first. Bile acid diarrhea is a specific biological condition with measurable markers. About 25-30% of people diagnosed with IBS-D actually have BAD. Treating it as IBS leads to ineffective care. Testing for BAD can change everything.
Can I take bile acid binders long-term?
Yes. Colesevelam is safe for long-term use. It’s not absorbed into the bloodstream, so it doesn’t affect other organs. The main concern is nutrient absorption-binders can reduce fat-soluble vitamins (A, D, E, K). If you’re on them long-term, get your vitamin levels checked yearly and consider a multivitamin taken 4 hours apart from the binder.
Does coffee make bile acid diarrhea worse?
Yes. Caffeine stimulates colonic motility by 15-20%, which pushes bile acids through your system faster. Even if your fat intake is low, coffee can trigger urgency and diarrhea. Try switching to decaf or herbal tea for a few weeks to see if it helps.
Why do I have greasy, pale stools with BAD?
When bile acids aren’t properly recycled, they don’t reach the small intestine to help digest fat. Undigested fat ends up in your stool, making it oily, pale, and hard to flush. This is a classic sign of bile acid malabsorption-not just diarrhea.
Can stress make bile acid diarrhea worse?
Stress doesn’t cause BAD, but it can worsen symptoms. Stress activates the gut-brain axis, speeding up colon contractions and increasing sensitivity. Managing stress through mindfulness, sleep, or therapy can help reduce flare frequency-even if you’re on medication.
What if binders don’t work?
If binders fail, talk to a specialist. You might need a higher dose, a different binder, or combination therapy. Some patients respond to bile acid synthesis inhibitors like elobixibat (available outside the U.S.) or FGF19 analogs in clinical trials. Genetic testing may also reveal why treatment isn’t working.






steffi walsh
19 November 2025OMG I’ve been dealing with this for YEARS and no one ever told me it could be BAD 😭 I started psyllium last week and my morning runs are down from 5 to 1. I feel like a new person. If you’re reading this and have IBS-D-just try it. No cost, no pills, just fiber. You’ve got nothing to lose.
Katelyn Sykes
20 November 2025Psyllium changed my life but I learned the hard way-don’t take it dry. I choked on a spoonful once and thought I was dying. Mix it with apple sauce or water. And drink like a gallon after. Also-don’t take it with your meds. I missed my thyroid pill for a week because I didn’t know. Lesson learned.
Gabe Solack
22 November 2025Just wanted to say thank you for this post. I’ve been on colesevelam for 6 months and it’s been a game changer. I used to avoid social events because I didn’t know when I’d have to run to the bathroom. Now I can go out to dinner without panic. 🙌 Also-yes, coffee is the devil. Switched to chamomile and my nights are finally quiet.
Riohlo (Or Rio) Marie
24 November 2025How quaint. You’re all treating this like some trendy wellness hack. Bile acid diarrhea isn’t a lifestyle tweak-it’s a physiological collapse of enterohepatic circulation, and you’re all just vibing with psyllium while ignoring the real issue: the pharmaceutical-industrial complex doesn’t want you to know how cheap and effective cholestyramine is. They’re pushing Welchol because it’s patentable. Meanwhile, the SeHCAT test? Still banned in the US because it’s ‘too cheap’ to profit from. Wake up. This is systemic medical neglect disguised as ‘personal responsibility.’
Kristina Williams
25 November 2025Wait so you’re saying the government is hiding this because of Big Pharma? I knew it. My cousin’s friend’s neighbor had this and they said the CDC told her to stop drinking milk because ‘it’s a toxin.’ Also I read on a forum that glyphosate causes bile acid malabsorption. I stopped eating bread and now I’m fine. Probably the wheat. Or the 5G. Or both.
Leilani O'Neill
26 November 2025It’s pathetic. People in Ireland used to know how to eat-real food, no nonsense. Now you’re all taking fiber powders and calling it medicine. Back in my day, if you had diarrhea, you drank tea, ate plain rice, and stopped being lazy. No binders. No apps. No ‘tracking.’ Just discipline. And you call this progress?
Gabriella Jayne Bosticco
26 November 2025I’m not a doctor but I’ve had this for 12 years. The C4 test was a lifesaver. My GP said ‘it’s probably IBS’ and I almost believed him. Then I found a GI who actually listened. If you’re reading this and you’ve been told ‘it’s all in your head’-go somewhere else. You deserve better. And yes, the binders suck but they’re worth it. I still hate the taste of cholestyramine but I’d rather have a normal life than a clean mouth.
Denny Sucipto
27 November 2025Just want to say to anyone reading this-don’t give up. I was on cholestyramine for a month, hated it, quit, went back to hell. Then I tried colesevelam. Still not tasty but it’s like chalk vs. sand. And psyllium? Best $8 I ever spent. You’re not broken. You just haven’t found the right combo yet. Keep going. You got this.
Bailey Sheppard
29 November 2025My mom had this after gallbladder removal. She didn’t even know what it was until her GI said ‘try Welchol.’ Two days later she said ‘I think I’m human again.’ I’m so glad this is getting more attention. So many people suffer in silence. Thank you for sharing the science and the real talk.
Iska Ede
29 November 2025So let me get this straight-you’re telling me I’ve been paying $400 a month for a drug that’s basically activated charcoal with a fancy name? And the real fix is… eating less bacon? Wow. I feel like I’ve been scammed by my own pancreas.
Yash Nair
30 November 2025India has been treating this for centuries with turmeric and ginger. You people are so obsessed with pills you forgot how to use food. I take 1 tsp turmeric with warm water every morning. No binders. No apps. Just ancient wisdom. Why are you all still using Western medicine when our grandmas knew better?
Conor McNamara
1 December 2025i think the bile acid thing is real but i also think the gov is using it to cover up the 5g towers in hospitals. they want us to think its our diet but its really the microwaves messing with our ileum. i tried the psyllium but it made my teeth feel funny. also i read on a blog that the sehcat test has a chip in it. i dont trust it. i just drink salt water now. its working.
Sarah Frey
3 December 2025Thank you for this meticulously researched and clinically grounded overview. The integration of diagnostic criteria, therapeutic modalities, and patient-reported outcomes represents a significant contribution to the literature on functional gastrointestinal disorders. I would respectfully suggest that future iterations consider including references to the 2022 ACG guidelines on bile acid malabsorption, as well as a brief discussion on the cost-effectiveness of serum C4 testing versus empirical binder trials in primary care settings. This is precisely the kind of evidence-based, compassionate communication that transforms patient care.