Introduction: Stress and Its Effects on the Body
The human body responds to stress in various ways. Some people might experience headaches or stomach aches, while others could experience more severe symptoms like high blood pressure or heart disease. However, one less recognized effect of stress is eye inflammation, an uncomfortable and sometimes painful condition. In this article, we will delve into the connection between stress and eye inflammation, aiming to shed some light on this underexplored issue.
Understanding Eye Inflammation
Eye inflammation, also known as uveitis, is a condition that involves swelling and irritation of the uvea, the middle layer of the eye. This condition can cause redness, pain, and blurred vision. In severe cases, it could even lead to loss of vision. There are different types of uveitis, depending on which part of the uvea is affected. It's important to understand that eye inflammation can be a symptom of an underlying disease or condition, including stress.
The Stress Response and Its Impact on the Eyes
When we encounter a stressful situation, our body goes into 'fight or flight' mode. This response involves various physiological changes, such as increased heart rate and blood pressure. It also causes a surge in cortisol, a hormone that can have a direct impact on various parts of the body, including the eyes. This surge in cortisol can cause inflammation in various parts of the body, including the uvea. This could explain why people under a lot of stress often complain about eye discomfort or vision problems.
Stress and Dry Eye Syndrome
Stress doesn't only lead to eye inflammation, but it can also cause dry eye syndrome. This condition occurs when your eyes don't produce enough tears or the right quality of tears to keep them lubricated. This can cause a stinging or burning sensation in your eyes, making them red and irritated. Studies suggest that stress can affect tear production, exacerbating the symptoms of dry eye syndrome.
Effects of Chronic Stress on Eye Health
While short-term stress might cause temporary discomfort or vision problems, chronic stress can have more serious effects on your eye health. Long-term stress can lead to conditions like glaucoma and age-related macular degeneration. These are serious eye conditions that can lead to vision loss if not treated promptly. Therefore, it's crucial to manage chronic stress to protect your eye health.
Managing Stress for Eye Health
Managing stress is not just beneficial for your overall health, but it's also crucial for maintaining good eye health. This can be done through various methods such as regular exercise, meditation, and deep breathing exercises. It's also important to have a healthy diet, as certain nutrients can help reduce inflammation and support eye health. If you're having trouble managing your stress levels, you might want to consider seeking professional help.
Getting Professional Help
If you're experiencing severe or persistent eye inflammation, it's important to seek professional help. A healthcare professional can provide a proper diagnosis and recommend suitable treatments. They can also help you find effective ways to manage stress if it's identified as the cause of your eye inflammation.
Conclusion: Stress and Eye Health
Eye health is often overlooked when discussing the effects of stress on the body. However, as we've discussed, stress can lead to various eye problems including eye inflammation and dry eye syndrome. Therefore, managing stress is crucial not just for your overall health, but also for maintaining good eye health. Remember, it's always better to prevent than to treat, so take good care of your eyes and try to manage stress before it becomes a problem.
References
For anyone interested in learning more about this topic, here are some references to scientific studies and articles that delve deeper into the relationship between stress and eye health.






abhi sharma
6 July 2023Oh great, another article telling me stress hurts my eyes, thanks for the groundbreaking revelation.
mas aly
6 July 2023I can see how overwhelming stress might translate into eye discomfort.
When cortisol spikes, inflammation can spread to delicate tissues like the uvea.
It makes sense that dry‑eye symptoms could worsen under pressure.
Managing stress with simple habits can be a real game‑changer for eye health.
Thanks for summarizing the science in an accessible way.
Abhishek Vora
6 July 2023The relationship between chronic cortisol elevation and ocular inflammation has been elucidated in numerous peer‑reviewed studies.
First, sustained activation of the hypothalamic‑pituitary‑adrenal axis results in systemic oxidative stress, which directly damages endothelial cells of the retinal vasculature.
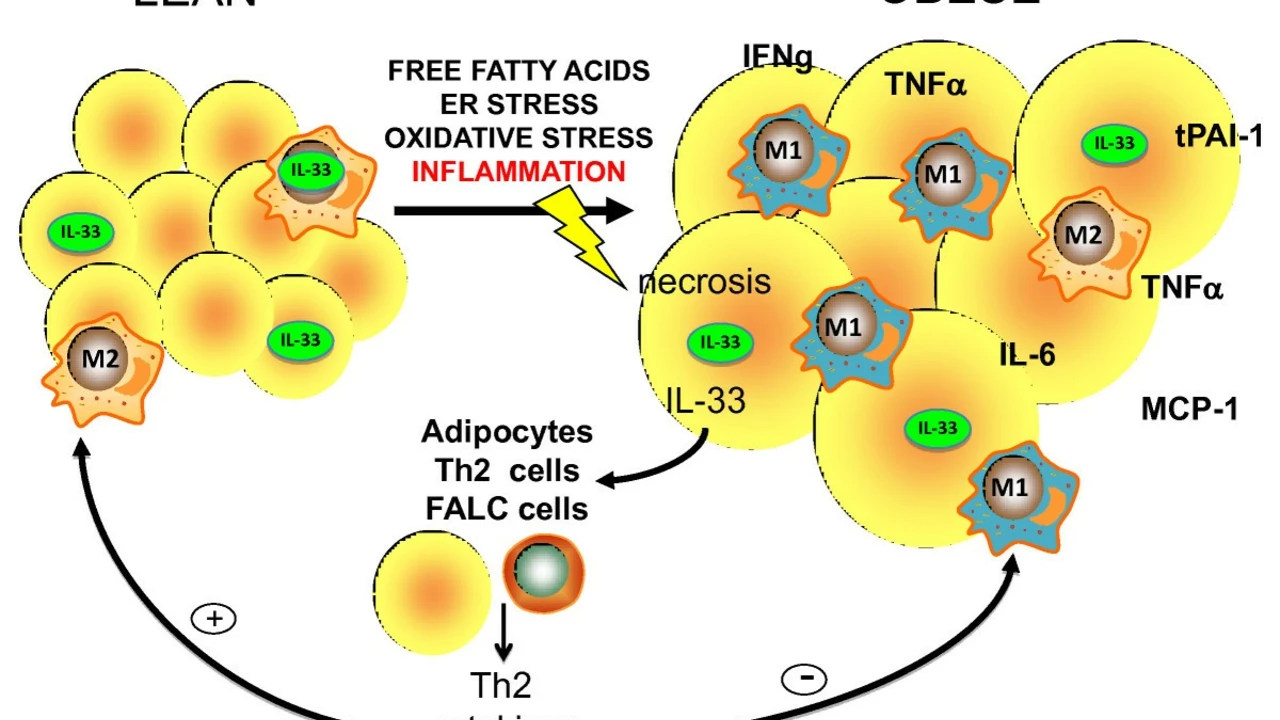
Second, inflammatory cytokines such as IL‑6 and TNF‑α, released during stress, cross the blood‑ocular barrier and incite uveitic processes.
Third, stress‑induced dysregulation of autonomic innervation reduces tear film stability, precipitating dry‑eye syndrome.
Moreover, experimental models demonstrate that glucocorticoid receptor agonism can paradoxically amplify local inflammation when administered chronically.
In clinical practice, patients presenting with unexplained uveitis often have a background of high‑job anxiety or unresolved psychological trauma.
A thorough psychosocial assessment should therefore accompany the ophthalmic work‑up.
Interventions such as cognitive‑behavioral therapy have shown measurable reductions in inflammatory markers.
Furthermore, dietary supplementation with omega‑3 fatty acids and lutein can mitigate oxidative damage.
Neglecting these adjunctive strategies risks progression to sight‑threatening complications.
It is also worth noting that stress can exacerbate comorbid conditions like hypertension, which themselves jeopardize retinal perfusion.
Hence, a multidisciplinary approach is not merely advisable but essential.
Patients who adopt regular mindfulness practices often report both subjective relief and objective improvement in tear breakup time.
In summary, the eye is not an isolated organ; it responds dynamically to systemic stressors.
Therefore, clinicians must address both the physiological and psychological dimensions to preserve visual function.
maurice screti
6 July 2023One must appreciate the sheer elegance with which endocrine perturbations cascade into ocular pathology; it is, frankly, a marvel of biological interconnectedness.
While the article offers a commendable overview, it scarcely grazes the profound epigenetic ramifications that chronic stress imprints upon retinal gene expression.
Consider, for instance, the up‑regulation of NF‑κB pathways, a subtle yet pivotal driver of vascular inflammation.
Moreover, the discourse neglects the socioeconomic dimensions that exacerbate stress‑related eye disease in underserved populations.
It would be remiss not to highlight the role of circadian rhythm disruption, another underexplored vector linking psychosocial strain to visual fatigue.
In an era where precision medicine beckons, integrating stress‑reduction protocols into ophthalmic care seems not just prudent but inevitable.
Thus, while the piece serves as a decent primer, the tapestry of causality extends far beyond its modest threads.
Abigail Adams
6 July 2023While the discussion is comprehensive, it inadequately addresses the hierarchy of causative factors, prioritizing stress over more salient etiologies such as autoimmune dysregulation.
Furthermore, the recommendation to "manage stress" lacks specificity, offering no actionable protocols for patients with refractory uveitis.
From a clinical standpoint, the omission of steroid-sparing agents is a notable oversight.
It is imperative to acknowledge that stress, albeit contributory, is seldom the primary catalyst for ocular inflammation.
Consequently, a more balanced framework that integrates immunomodulatory therapy alongside lifestyle interventions would be advisable.
Overall, the article serves as a cursory overview but falls short of delivering the nuanced guidance required for effective management.
Belle Koschier
6 July 2023I appreciate the balanced perspective and think emphasizing collaborative care between ophthalmologists and mental‑health professionals could really benefit patients.
Small, practical steps like regular breaks from screens and mindfulness exercises are simple yet powerful tools.