Introduction: Understanding Lisinopril and Mental Health
Lisinopril is a medication commonly prescribed to treat high blood pressure and heart failure. While it is primarily used for cardiovascular health, recent studies have suggested that it may also have an impact on mental health. In this article, we will explore the various ways in which Lisinopril may affect mental wellbeing, including its potential benefits and risks.
The Connection Between Cardiovascular Health and Mental Health
Before we delve into the effects of Lisinopril on mental health, it is essential to understand the connection between cardiovascular health and mental wellbeing. Poor cardiovascular health has been linked to numerous mental health issues, such as depression, anxiety, and cognitive decline. This is because the heart and brain are closely connected, and any damage to the cardiovascular system can have a direct impact on the brain's function and overall mental health.
Lisinopril and Its Impact on Anxiety
One of the potential mental health benefits of Lisinopril is its possible effect on anxiety levels. Studies have shown that individuals with high blood pressure often experience increased anxiety levels. By lowering blood pressure, Lisinopril may help alleviate anxiety symptoms in some individuals. However, more research is needed to confirm this potential benefit and determine the extent to which Lisinopril may affect anxiety.
Lisinopril and Its Role in Depression
Depression is another mental health issue that may be impacted by Lisinopril treatment. Some research has suggested that individuals with high blood pressure are at a higher risk of developing depressive symptoms. By effectively managing blood pressure, Lisinopril may help reduce the risk of depression in some individuals. However, it is important to note that the relationship between Lisinopril and depression is not yet fully understood, and more studies are needed to determine the true impact of this medication on depressive symptoms.
Cognitive Function and Lisinopril
Another area of mental health that may be affected by Lisinopril is cognitive function. High blood pressure has been linked to cognitive decline and an increased risk of dementia. By reducing blood pressure, Lisinopril may help protect cognitive function and reduce the risk of cognitive decline in individuals with hypertension. However, more research is required to fully understand the relationship between Lisinopril and cognitive function.
Potential Side Effects of Lisinopril on Mental Health
While Lisinopril may have some potential mental health benefits, it is also important to be aware of the potential side effects of this medication. Some individuals may experience adverse mental health effects while taking Lisinopril, such as mood swings, irritability, or even depression. It is important to monitor your mental health while taking Lisinopril and speak with your healthcare provider if you notice any concerning changes in your mental wellbeing.
Interactions Between Lisinopril and Other Medications
When considering the impact of Lisinopril on mental health, it is also crucial to be aware of potential interactions with other medications. Some medications, such as antidepressants or anti-anxiety medications, may interact with Lisinopril and affect its efficacy or cause additional side effects. It is essential to discuss all medications you are taking with your healthcare provider to ensure that there are no harmful interactions.
The Importance of Monitoring Mental Health While Taking Lisinopril
As with any medication, it is important to monitor your mental health while taking Lisinopril. Keep track of any changes in your mood, anxiety levels, or cognitive function, and discuss these changes with your healthcare provider. They can help determine if these changes are related to Lisinopril or if other factors may be contributing to your mental health concerns.
Alternative Treatments for High Blood Pressure and Mental Health
If you are concerned about the potential impact of Lisinopril on your mental health, it is important to discuss alternative treatment options with your healthcare provider. There are several other medications and lifestyle changes that can help manage high blood pressure and improve mental wellbeing. These may include other blood pressure medications, exercise, dietary changes, and stress management techniques.
Conclusion: Weighing the Benefits and Risks of Lisinopril for Mental Health
In conclusion, Lisinopril may have both positive and negative impacts on mental health. While it may help reduce anxiety, depression, and cognitive decline in some individuals, others may experience adverse side effects or medication interactions. It is essential to monitor your mental health while taking Lisinopril and discuss any concerns with your healthcare provider. Together, you can weigh the potential benefits and risks of this medication and determine the best course of treatment for your unique needs.





Christopher Eyer
29 April 2023While the article attempts to associate Lisinopril with mental health outcomes, the evidnce presented is largely anecdotal and fails to establish a causual relationship. Moreover, the cardiologic benefits of the drug are well‑documented, whereas any psychologic impact remains speculative at best.
Mike Rosenstein
29 April 2023It is important to recognize that individual responses to Lisinopril can vary, and clinicians should adopt a patient‑centered approach when monitoring both blood pressure and mood. Providing clear guidance and regular follow‑up can help mitigate potential side effects while enhancing overall wellbeing.
Ada Xie
29 April 2023The manuscript contains several grammatical oversights; for instance, the phrase “may also have an impact on mental health” should be rendered as “may also impact mental health.” Additionally, consistency in tense throughout the discussion would improve readability.
Stephanie Cheney
29 April 2023Considering the interconnectedness of cardiovascular and mental health, encouraging lifestyle modifications such as regular exercise and stress‑reduction techniques can complement pharmacotherapy. These supportive measures often enhance therapeutic outcomes without imposing additional medication burdens.
Georgia Kille
29 April 2023Keep tracking your mood and blood pressure-consistency is key! 😊
Jeremy Schopper
29 April 2023Indeed, Lisinopril’s primary function is to modulate the renin‑angiotensin system, thereby reducing systemic vascular resistance, and consequently lowering arterial pressure; however, clinicians should remain vigilant for neuropsychiatric manifestations, such as irritability or mood fluctuations, that may arise in susceptible patients, and adjust treatment protocols accordingly, ensuring a holistic approach to cardiovascular and mental health management.
liza kemala dewi
29 April 2023The relationship between antihypertensive agents and neurocognitive function has long intrigued clinicians and philosophers alike. From a mechanistic standpoint, Lisinopril attenuates the activity of angiotensin‑converting enzyme, thereby diminishing the production of angiotensin II, a peptide implicated not only in vasoconstriction but also in neuroinflammation. Neuroinflammation, as current research suggests, plays a pivotal role in the etiology of depressive disorders and cognitive decline. Consequently, one might hypothesize that by curbing this inflammatory cascade, Lisinopril could exert a protective effect on the brain. Empirical studies, however, present a nuanced picture; some randomized trials have reported modest improvements in anxiety scores, while others have found no statistically significant difference compared with placebo. This heterogeneity may reflect variations in study populations, dosing regimens, and the sensitivity of psychometric instruments employed. Moreover, the psychosocial context of each patient-encompassing stress levels, social support, and concurrent therapies-cannot be ignored when interpreting these outcomes. It is also worth noting that the blood‑brain barrier exhibits selective permeability, and the extent to which Lisinopril penetrates this barrier remains a matter of scientific debate. Should the drug achieve sufficient central concentrations, its influence on neurotransmitter modulation could be more pronounced. Conversely, peripheral effects, such as improved cerebral perfusion resulting from better blood pressure control, may indirectly benefit cognitive function. From a philosophical perspective, we are reminded that causation in medicine is seldom linear; rather, it resembles a symphony of interacting variables. Therefore, attributing mental health changes solely to a single pharmacologic agent oversimplifies the complex adaptive systems at play. Clinicians are thus urged to adopt a biopsychosocial framework that integrates pharmacotherapy with lifestyle interventions and mental health support. In practice, regular monitoring of mood, sleep quality, and cognitive performance can help discern whether Lisinopril contributes positively or negatively to a patient’s overall wellbeing. Ultimately, the decision to continue or discontinue the medication should be individualized, based on a careful weighing of cardiovascular benefits against potential neuropsychiatric effects.
Jay Jonas
29 April 2023Yo, man, i get the whole over‑the‑top vibe, but honestly, Lisinopril might just be chillin’ in the bloodstream without messin’ with your head-unless you’re already on a rollercoaster of stress, then who knows, right?
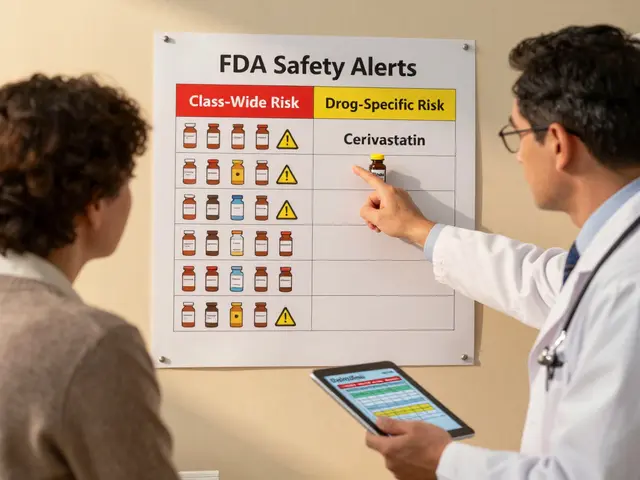
Liam Warren
29 April 2023From a cardiovascular risk stratification standpoint, integrating Lisinopril into a polypharmacy regimen necessitates vigilant pharmacodynamic monitoring to preempt any neuro‑psychiatric signal spillover, especially when beta‑blockers or SSRIs are co‑prescribed.
Brian Koehler
29 April 2023Indeed, the interplay between hemodynamic modulation and cerebral neurotransmission can be as vibrant as a kaleidoscopic sunrise; nevertheless, clinicians must remain astutely aware of the subtle nuances that may emerge when the renin‑angiotensin axis is tweaked-lest we overlook the quiet whispers of mood alteration.