Fungal Infection Risk Calculator
Personal Risk Assessment
This calculator helps you assess your risk of developing fungal-related sores based on factors mentioned in the article. Enter information about your health and lifestyle to get a personalized risk assessment.
Your Risk Assessment
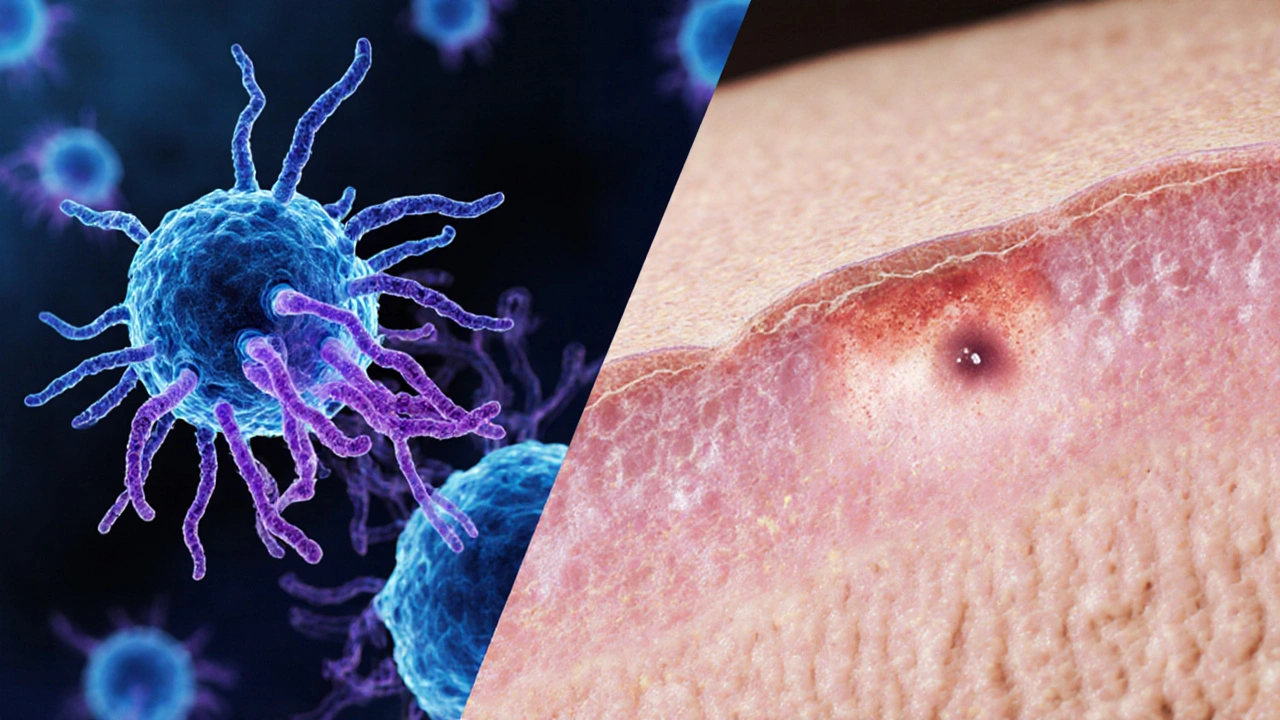
When a harmless‑looking rash turns into a painful sore, many people wonder if a hidden fungus is to blame. Understanding the link between fungal infections and sore development can stop the problem early and keep your skin healthy.
Key Takeaways
- Fungal infections such as candidiasis and dermatophyte infections are common triggers for skin sores.
- Typical sore‑causing fungi include Candida albicans - a yeast that thrives in warm, moist areas - and dermatophytes, a group of molds that feed on keratin.
- Risk factors like diabetes, a weakened immune system, and prolonged moisture increase the chance of fungal‑related sores.
- Early diagnosis (KOH prep, cultures) and targeted antifungal treatment usually clear the infection and prevent scar‑forming sores.
- Good hygiene, breathable clothing, and prompt treatment of minor skin issues are the best defenses.
What Exactly Is a Fungal Infection?
Fungal infection is a condition where fungi - yeasts, molds, or dermatophytes - invade skin, nails, or mucous membranes, causing irritation, inflammation, and sometimes tissue breakdown. While many fungi live harmlessly on the body, an imbalance or breach in the skin barrier lets them multiply, leading to symptoms that range from mild itching to open sores.
How Sores Form From Fungal Activity
When fungi colonise a spot, they release enzymes that digest keratin and other proteins. This enzymatic attack damages the outer skin layers, creating micro‑ulcers. If the immune response is insufficient or the area stays moist, the tiny lesions merge into larger, painful sores.

Common Fungi That Cause Sores
Not all skin fungi produce the same kind of sore. Below are the main culprits:
- Candida albicans - a yeast that usually causes oral thrush or vaginal yeast infections but can also lead to intertriginous (skin‑fold) sores when moisture is trapped.
- Dermatophytes - a family of keratin‑eating molds that include species causing athlete’s foot, ringworm, and jock itch. Their growth creates scaly borders that can break down into open lesions.
- Tinea corporis - also known as “ringworm of the body,” presents as a ring‑shaped rash that may ulcerate if scratched.
- Athlete’s foot (tinea pedis) - often starts between the toes as a macerated, itchy patch and can develop painful fissures or sores.
- Ringworm (tinea capitis) - affects the scalp; the infected hair follicles can become inflamed and break, leaving crusted sores.
Risk Factors That Boost the Chances of Sores
Even the most resilient skin can succumb when certain conditions exist:
- Chronic moisture - sweaty feet, occlusive clothing, or prolonged bathing.
- Underlying health issues - diabetes, HIV, or any condition that weakens the immune system.
- Skin trauma - cuts, abrasions, or even aggressive scratching.
- Antibiotic use - broad‑spectrum antibiotics can disrupt normal flora, allowing fungi to overgrow.
- Age - infants and elderly people have thinner skin and reduced immunity.
How to Diagnose a Fungal‑Related Sore
Early, accurate diagnosis stops a sore from worsening. Clinicians typically follow these steps:
- Visual examination: Characteristic ring‑shaped or macerated lesions hint at specific fungi.
- KOH (potassium hydroxide) prep: A skin scraping mixed with KOH dissolves skin cells, revealing fungal hyphae or yeast under a microscope.
- Culture: Samples placed on Sabouraud agar grow the organism for precise identification.
- Wood’s lamp: Certain dermatophytes fluoresce under UV light, aiding quick detection.

Treatment Options: From Creams to Pills
Choosing the right therapy depends on the fungus type, sore severity, and patient health.
| Infection | Typical Location | Appearance | First‑line Treatment | When to See a Doctor |
|---|---|---|---|---|
| Candida albicans | Skin folds, oral cavity, genital area | Red, moist patches that may ooze | Topical azoles (clotrimazole) or oral fluconazole for extensive disease | Rapid spread, fever, or diabetic patient |
| Dermatophytes (tinea pedis) | Between toes, soles | Scaling, maceration, fissures | Topical terbinafine or tolnaftate for 2-4 weeks | Painful fissures, swelling, or secondary bacterial infection |
| Tinea corporis | Arms, torso, legs | Ring‑shaped, raised border, central clearing | Topical allylamines (naftifine) or oral itraconazole if extensive | Lesion >5cm, multiple sites, or immune‑compromised |
| Ringworm of scalp (tinea capitis) | Scalp | Hair loss patches, scaling, crusted sores | Oral griseofulvin or terbinafine for 4-6 weeks | Persistent hair loss, large crusted plaques |
Topical agents work well for localized infections, but when sores are deep, widespread, or involve the nails, oral antifungals become necessary. Completing the full medication course is crucial; stopping early often leads to recurrence.
Preventing Fungal‑Induced Sores
Prevention is easier than cure. Adopt these habits:
- Keep skin dry - towel off thoroughly after showers, especially between toes.
- Wear breathable footwear - opt for leather or mesh shoes and change socks daily.
- Avoid sharing personal items - towels, razors, and nail clippers can spread spores.
- Control blood sugar - good diabetes management reduces fungal overgrowth.
- Use antifungal powders for high‑risk areas - especially if you sweat heavily.
When to Seek Professional Care
If a sore:
- Persists longer than two weeks despite over‑the‑counter creams,
- Shows signs of infection - increasing redness, warmth, pus, or fever,
- Appears on the face, genitals, or near the eyes,
- Is associated with diabetes, HIV, or other immune‑suppressing conditions,
- Is painful enough to limit daily activities,
schedule a visit. Early prescription therapy can spare you from scarring and secondary bacterial infection.
Frequently Asked Questions
Can a fungal infection cause a sore without visible rash?
Yes. Some yeast infections begin as hidden inflammation in skin folds; the sore may appear as a small ulcer before the surrounding redness becomes noticeable.
How long does it take for a fungal sore to heal after treatment?
Topical therapy usually clears visible symptoms in 2-4 weeks, but the underlying fungus may need up to 6 weeks to disappear completely. Oral medications can take 4-8 weeks for full resolution.
Are over‑the‑counter antifungal creams enough for all sore‑causing fungi?
They work for mild, localized dermatophyte infections. For extensive, recurrent, or deep‑seated sores (especially in diabetics), prescription‑strength creams or oral agents are often required.
Can I prevent fungal sores by using probiotics?
Probiotics may help maintain a healthy microbial balance, but they are not a guaranteed preventive measure. Good hygiene and moisture control remain the primary defenses.
Is it safe to treat a fungal sore with home remedies like tea tree oil?
Tea tree oil has antifungal properties, but concentrations vary. It can irritate sensitive skin and may not clear deeper infections. Use it only as adjunct to proven treatments, and stop if irritation occurs.
Understanding how fungal invaders turn into sore‑forming lesions empowers you to spot problems early, act decisively, and keep your skin barrier intact. Stay dry, clean, and alert - your skin will thank you.






Anna-Lisa Hagley
14 October 2025Fungal sores are just another reminder that our bodies are ecosystems we constantly neglect.
A Walton Smith
21 October 2025Yeah whatever.
Theunis Oliphant
28 October 2025It is a disgrace that modern society tolerates the proliferation of fungal infections as if they were a mere inconvenience. The very existence of persistent sores on the skin signals a failure to uphold basic hygienic standards. One must first acknowledge that the skin functions as a vital barrier, a shield against the invasive world of microscopic pathogens. When this barrier is compromised, the opportunistic fungi seize the moment, turning a banal irritation into a chronic affliction. The underlying causes-diabetes, immunosuppression, chronic moisture-are not excuses but indictments of personal neglect. It is incumbent upon each individual to conduct a rigorous self‑assessment, much like the calculator presented in the article, and to act accordingly. The recommended preventive measures-keeping skin dry, wearing breathable footwear, avoiding shared personal items-are elementary yet often ignored. Moreover, the therapeutic hierarchy outlined, from topical agents to systemic antifungals, reflects a logical escalation that must be respected. Patients should never abandon a prescribed course prematurely, for doing so invites recurrence and deeper invasion. The moral imperative extends beyond the individual; healthcare providers must educate their patients with uncompromising clarity. In clinical practice, one should stringently monitor for signs of secondary bacterial infection, which exacerbate the situation. The article’s FAQ section aptly underscores that over‑the‑counter creams are insufficient for extensive disease, a fact that is frequently overlooked. Probiotics, while popular, cannot substitute for rigorous moisture control and diligent skin care. Even alternative remedies such as tea tree oil must be approached with caution, lest they cause further irritation. Ultimately, the battle against fungal‑induced sores is a test of personal responsibility, medical diligence, and societal awareness. Let us therefore reject complacency and embrace a disciplined approach to skin health.
India Digerida Para Occidente
4 November 2025I get where you’re coming from, but I also think it’s important to recognize that many people simply lack access to proper dermatological care, which makes strict self‑discipline harder to achieve. Offering community clinics and affordable antifungal options can bridge that gap while still emphasizing good hygiene.
Andrew Stevenson
12 November 2025From a clinical standpoint, the pathophysiology of dermatophyte infections involves keratinolysis mediated by secreted proteases that degrade the stratum corneum, creating a niche for lesion formation. The risk calculator in the article essentially quantifies exposure to key predisposing variables-hyperglycemia, immunosuppression, occlusion, trauma, antibiotic pressure, and age-related skin changes. When the aggregate score exceeds a threshold, clinicians should consider initiating a topical azole such as clotrimazole 1% twice daily, progressing to an oral allylamine like terbinafine 250 mg daily for 2–4 weeks in extensive cases. Pharmacokinetic considerations dictate monitoring hepatic function for prolonged systemic therapy, especially in geriatric patients. Adjunctive measures, including foot powder with antifungal agents (e.g., miconazole) and moisture‑wicking socks, serve to reduce the local microclimate that favors fungal proliferation. It’s also advisable to perform a KOH preparation or fungal culture to confirm the etiologic species, which can guide therapeutic selection-Trichophyton versus Candida may respond differently to itraconazole versus fluconazole. Lastly, patient education on avoiding shared footwear, regular nail trimming, and prompt treatment of intertriginous moisture can markedly decrease recurrence rates.
Kate Taylor
19 November 2025That’s a solid breakdown-especially the part about confirming the species before jumping straight to oral meds. I’d add that keeping the affected area exposed to air, when possible, speeds up drying and helps the topical agents work better.
Hannah Mae
26 November 2025People act like fungal sores are always a sign of personal failure, but sometimes it’s just bad luck.
Iván Cañas
3 December 2025True, environmental humidity can play a huge role, especially in coastal regions where moisture is constant.
Jen Basay
10 December 2025Exactly! 😊 Staying in air‑conditioned rooms and using absorbent foot powders can make a noticeable difference.
Hannah M
17 December 2025Great tips, everyone! 🙌 Keeping the skin dry and using proper antifungal powders really is the easiest preventive step.
Poorni Joth
24 December 2025Honestly the problem is that ppl dont take personal hygiene seriously and just ignore simple advices, its irresponsible.
Yareli Gonzalez
31 December 2025Remember, small daily habits add up to big health gains.
Alisa Hayes
7 January 2026Absolutely, Yareli. Consistently drying between toes after a shower, swapping out socks daily, and checking for early signs of irritation can prevent a full‑blown infection. Even a quick glance in the mirror each morning can catch a red patch before it spreads.
Mariana L Figueroa
14 January 2026Keep it simple use a daily antifungal foot spray and change shoes regularly