What Is Topical Medication Allergy?
It’s not just a rash. If you’ve applied a cream or ointment for eczema, a cut, or a bug bite - and instead of getting better, your skin gets redder, itchier, and starts to blister - you might be having an allergic reaction to the medication itself. This is called allergic contact dermatitis, and it’s more common than most doctors admit.
Unlike irritation from soap or water, which burns or stings right away, allergic reactions to topical drugs take time. They usually show up 24 to 72 hours after use. The skin doesn’t just react - it remembers. Once you’ve had one reaction, even a tiny amount of that same ingredient can trigger it again, sometimes years later.
It’s not rare. About 1 in 6 people who get patch-tested for stubborn rashes turn out to be allergic to something in their topical medicine. And the biggest culprits? Antibiotics like neomycin and bacitracin, corticosteroids like hydrocortisone and triamcinolone, local anesthetics like benzocaine, and even over-the-counter pain creams with ketoprofen.
Why Your ‘Treatment’ Is Making Things Worse
Here’s the cruel twist: the very thing meant to heal your skin can be the reason it won’t heal.
Think about it. You have eczema. Your doctor prescribes a hydrocortisone cream. You use it daily. After a week, the redness spreads. The itching gets worse. You think you’re using it wrong - maybe you need more. So you apply it again. And again. Until your skin starts to crack, weep, or peel.
That’s not eczema flaring. That’s your body rejecting the steroid.
Studies show that 0.5% to 2.2% of people using topical corticosteroids develop an allergy to them. That means in a clinic seeing 1,000 patients with eczema, 5 to 22 of them are being treated with the exact thing making their condition worse. And most doctors don’t suspect it.
Dr. Erin Warshaw, former president of the American Contact Dermatitis Society, says nearly half of these cases are misdiagnosed at first because clinicians assume the treatment can’t be the problem. But it can. And it often is.
What Medicines Cause the Most Allergies?
Not all topical drugs are created equal when it comes to triggering allergies. Some are far more likely to cause reactions than others.
- Neomycin - Found in triple antibiotic ointments, wound sprays, and even some ear drops. It shows up in nearly 1 in 10 positive patch tests.
- Bacitracin - Often paired with neomycin. Also triggers reactions in about 7.5% of allergic patients.
- Hydrocortisone - The most common OTC steroid. Belongs to Group A corticosteroids, which have a high rate of cross-reactivity. If you’re allergic to this, you may react to other steroids too.
- Benzocaine - Used in numbing creams for hemorrhoids, sunburns, and teething gels. Causes reactions in about 2% of patch-tested patients.
- Ketoprofen - A topical NSAID used for muscle pain. Less common but highly reactive, especially in people with sensitive skin.
What’s surprising? Even “natural” ingredients like tea tree oil, lanolin, and coconut oil - often marketed as gentle - can trigger allergic contact dermatitis. And many people don’t realize these are in their prescriptions or moisturizers.
How Do You Know It’s an Allergy - Not Just Irritation?
There’s a big difference between irritant contact dermatitis and allergic contact dermatitis.
Irritant reactions happen to anyone if the substance is strong enough or used too long. Think of dish soap on your hands. It burns. It dries. It peels. That’s irritation. It doesn’t need your immune system to be involved.
Allergic reactions are different. They only happen to people who’ve been sensitized before. Your body learned to recognize the substance as a threat. Now, even a tiny amount triggers an immune response. That’s why you might use a cream for months with no problem - then suddenly, one day, your skin explodes.
Here’s how to tell:
- Location matters: Allergic rashes often appear where you applied the product - but sometimes spread beyond it. Irritant rashes stay exactly where you rubbed it on.
- Timing matters: Allergic reactions take 1-3 days to appear. Irritation shows up in minutes or hours.
- Pattern matters: Allergic dermatitis often looks like a defined shape - maybe even the outline of the bandage or the shape of the tube you squeezed it from.
And here’s the kicker: up to 20% of people who think they have a medication allergy actually have irritant dermatitis. That’s why testing is so important.

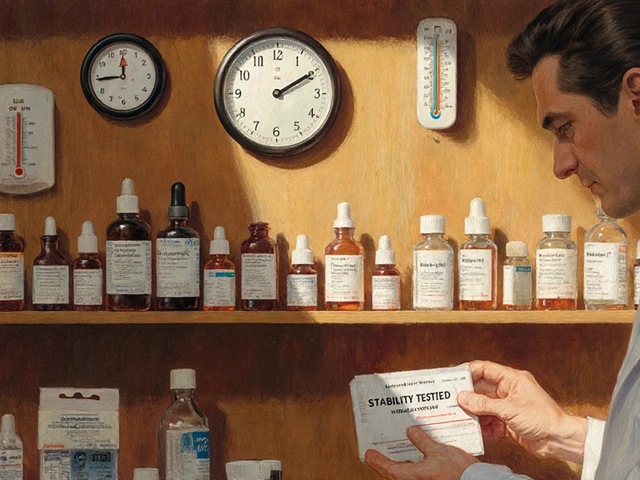
How Patch Testing Works - And Why You Need It
If you’ve had the same rash for months and nothing helps, it’s time for patch testing.
This isn’t a skin prick test like for peanut allergies. It’s a slow, careful process. Tiny amounts of 50-100 common allergens - including 20+ topical drugs - are placed on patches, stuck to your back, and left for 48 hours. You come back at 48 and 96 hours for readings.
At 48 hours, your doctor looks for redness, swelling, or tiny blisters. At 96 hours, they check again - because some reactions take longer to show up.
It’s not perfect, but it works in about 70% of cases when done right. And it’s the only way to know for sure what’s causing your rash.
Most dermatologists don’t offer it. But if you’ve tried three different creams and your skin keeps getting worse, ask for it. You have a right to know what’s triggering your body.
How to Treat Allergic Contact Dermatitis
Once you know what you’re allergic to, the first rule is simple: stop using it.
But stopping isn’t always easy. If you’ve been using a steroid cream for years, your skin may have gotten dependent on it. Suddenly stopping can cause rebound redness - called steroid withdrawal. That’s not an allergy. That’s your skin reacting to the loss of suppression.
Here’s what actually works:
- Stop the allergen: Remove every product containing the culprit ingredient - including lotions, sunscreens, and even hair products. Read labels. Use the American Contact Dermatitis Society’s mobile app to scan products.
- Use a gentle cleanser: Avoid soaps. Use fragrance-free, non-foaming cleansers like Cetaphil or Vanicream.
- Apply a low-potency steroid if needed: For mild cases, 0.5-1% hydrocortisone can help. But if you’re allergic to hydrocortisone, skip it. Use desonide (Desowen) instead - it’s weaker and safer for the face and groin.
- Try calcineurin inhibitors: Pimecrolimus (Elidel) and tacrolimus (Protopic) are non-steroid creams that calm the immune response. They work for 60-70% of patients with medication-induced dermatitis. Side effect? Burning at first - but it fades.
- For severe cases, take oral steroids: If more than 20% of your skin is affected, your doctor may prescribe prednisone. Symptoms often improve within 12-24 hours. But taper slowly - don’t stop cold.
Don’t rush back to steroids just because your skin looks better. The goal is to break the cycle - not replace one trigger with another.
What to Do If You’re Allergic to Steroids
Not all steroids are the same. Corticosteroids are grouped into six classes (A-F) based on chemical structure. If you’re allergic to Group A (like hydrocortisone), you might still tolerate Group B (triamcinolone) or Group D (methylprednisolone aceponate).
That’s why patch testing doesn’t just tell you what to avoid - it tells you what you can still use. One study showed that following this classification system reduces treatment limitations by 65%.
So if you’ve been told you’re allergic to all steroids - you’re probably wrong. Ask for a full allergy panel that includes steroid groups. You might have more options than you think.

How Long Does It Take to Get Better?
Most people start feeling relief within 48-72 hours after removing the allergen. But full healing takes time.
With proper avoidance and treatment, 89% of chronic cases clear up completely within four weeks. Without identifying the trigger, only 32% improve - even with strong medications.
On average, patients see 3.2 doctors before getting the right diagnosis. Some wait six months or longer. That’s why it’s so critical to speak up: “I think the medicine is making this worse.”
Don’t wait for your doctor to ask. Bring your products. Show them your rash. Say: “I’ve tried everything. I need patch testing.”
What’s New in Treatment and Prevention
The field is changing fast.
In 2023, researchers at Johns Hopkins found that diluting topical medications 10 times during patch testing cuts false negatives from 32% to just 9%. That’s huge - especially for people with broken skin who used to test negative but still reacted in real life.
Also new: the “Topical Medication Allergy Score,” a 12-point checklist used in Europe that boosts diagnostic accuracy from 65% to 89%. And the NIH just funded $4.7 million to develop blood tests that could predict who’s at risk before they even use a cream.
On the product side, new barrier creams are in clinical trials that block allergens from penetrating the skin by 73%. These aren’t moisturizers - they’re protective shields you apply before your usual cream.
And in Australia, where I live, the Therapeutic Goods Administration now requires full ingredient listing on all topical prescriptions. That’s helping doctors spot hidden allergens faster.
Real Stories, Real Impact
One woman on Reddit shared that she’d been using hydrocortisone cream for eczema for 10 years. When her face started burning and peeling, she thought she was allergic to everything. She avoided all creams. Her skin got worse. Only after patch testing did she learn: she was allergic to hydrocortisone - and had been using it daily for a decade.
Another man used Neosporin on every cut. When his forearm turned red and itchy, he blamed his job. He changed careers. Still no improvement. Patch test revealed neomycin allergy. He switched to plain petroleum jelly. Within two weeks, his skin cleared.
These aren’t rare cases. They’re the rule.
What You Can Do Today
- Stop using any cream that makes your skin worse - even if it’s “prescribed.”
- Write down every topical product you’ve used in the last 3 months - including OTC creams, sunscreens, and makeup.
- Bring them to your dermatologist. Say: “I think one of these is causing my rash.”
- Ask for patch testing if your rash won’t go away after 2-3 weeks.
- Don’t assume steroids are safe just because they’re common. They’re the #1 cause of drug allergies in topical form.
Your skin is a mirror. When it reacts, it’s not broken - it’s telling you something. Listen to it.
Can you be allergic to hydrocortisone cream?
Yes. Hydrocortisone is one of the most common causes of topical medication allergies. It’s in many over-the-counter creams and even some prescription formulas. If your rash gets worse after using it, or spreads beyond where you applied it, you could be allergic. Patch testing is the only way to confirm it.
How long does contact dermatitis last after stopping the allergen?
Itching usually improves within 48-72 hours. Redness and swelling fade over 1-2 weeks. Full skin healing can take 2-4 weeks. But if you keep using the allergen - even accidentally - the rash will return or get worse. Avoidance is the key.
Is patch testing painful?
No. It’s not a needle or a scratch. Small patches with allergens are taped to your back for 48 hours. You might feel slight itching or warmth, but no pain. You can shower normally. Just avoid scratching the area. The results are read by a trained professional at 48 and 96 hours.
Can you outgrow a topical medication allergy?
No. Once your immune system has reacted to a substance, it remembers it. Even if you haven’t used the product for years, re-exposure can trigger a reaction again. Avoidance is lifelong.
Are natural or organic topical products safer?
Not necessarily. Many plant-based ingredients - like tea tree oil, lanolin, balsam of Peru, and coconut oil - are common allergens. “Natural” doesn’t mean non-reactive. In fact, some botanicals cause more allergies than synthetic drugs. Always check ingredients, even on “gentle” labels.
What should I use instead of antibiotic ointments?
For minor cuts and scrapes, plain petroleum jelly (Vaseline) is often the best choice. It keeps the wound moist, prevents infection, and doesn’t contain allergens like neomycin or bacitracin. For deeper wounds or signs of infection, see a doctor - don’t self-treat with OTC creams.






Sheila Garfield
31 January 2026I used hydrocortisone for years thinking it was helping my eczema-turns out it was making everything worse. My skin finally calmed down only after I stopped everything and did patch testing. Best decision ever.
Shawn Peck
2 February 2026Stop using creams. Just use Vaseline. Done. No more drama. No more allergies. Simple.
April Allen
3 February 2026The immunological memory aspect here is fascinating. Allergic contact dermatitis isn't just a surface reaction-it's a T-cell-mediated epigenetic imprint. Once sensitized, the dendritic cells retain antigen-presenting memory in lymphoid tissue, which explains why re-exposure-even decades later-triggers a full-blown Type IV hypersensitivity. This is why avoidance isn't optional; it's biological imperative. The patch test isn't a luxury-it's a diagnostic gold standard that's been underutilized for decades because of clinical inertia.
Jason Xin
3 February 2026I used to roll my eyes at people who said their 'natural' lotion made them break out. Then I got a rash from tea tree oil. Now I read every ingredient like it's a contract. Turns out 'natural' just means more plant stuff your body might hate.
Lily Steele
4 February 2026I wish I'd known this sooner. I went to three doctors who just gave me stronger steroids. My skin was screaming and no one listened. Patch testing saved me. Don't be afraid to ask for it.
Kelly Weinhold
5 February 2026I used Neosporin on every little scrape for years like it was magic fairy dust. Then one day my arm looked like a crime scene. I thought it was stress or my job or the weather. Turns out? Neomycin. I switched to plain Vaseline and within two weeks my skin looked like it had never been touched by a tube of antibiotic cream. I feel like a new person. Also, I now read labels like I'm decoding a spy novel. No more guessing. No more suffering.
calanha nevin
7 February 2026The clinical data presented here is robust and aligns with current dermatological guidelines. Allergic contact dermatitis remains underdiagnosed due to diagnostic bias favoring irritant etiologies. Patch testing with extended reading at 96 hours significantly improves sensitivity. Furthermore, the use of dilution protocols to mitigate false negatives in compromised skin barriers represents a paradigm shift in allergen detection. Clinicians must prioritize this modality over empirical steroid escalation.
Lisa McCluskey
7 February 2026I used to think if it was in a drugstore, it was safe. Then I got a reaction from a 'gentle' baby cream with lanolin. Now I check every product on the ACD app. It's a habit now. Small effort. Big payoff.
owori patrick
8 February 2026In Nigeria, we use a lot of herbal pastes and oils for skin problems. Many people don't realize they're allergic until it's too late. This article is a wake-up call. We need more education here about what 'natural' really means.
Claire Wiltshire
10 February 2026Thank you for sharing this comprehensive overview. As a healthcare provider, I routinely counsel patients on ingredient awareness, particularly with topical agents. The prevalence of allergic reactions to commonly prescribed corticosteroids and antibiotic combinations is alarmingly high and often misattributed. I encourage all patients with persistent dermatitis to request patch testing-not as a last resort, but as a first-line diagnostic step. Knowledge is the most effective treatment.