Quit Smoking and Congestive Heart Failure: What You Need to Know
When working with Quit Smoking, the act of stopping tobacco use to protect your health. Also known as smoking cessation, it plays a crucial role for people with Congestive Heart Failure, a condition where the heart cannot pump blood efficiently and overall Cardiovascular Health, the well‑being of the heart and blood vessels. Addressing Nicotine Addiction, the physical and psychological dependence on nicotine often requires Smoking Cessation Programs, structured support such as counseling, medication, or digital tools.
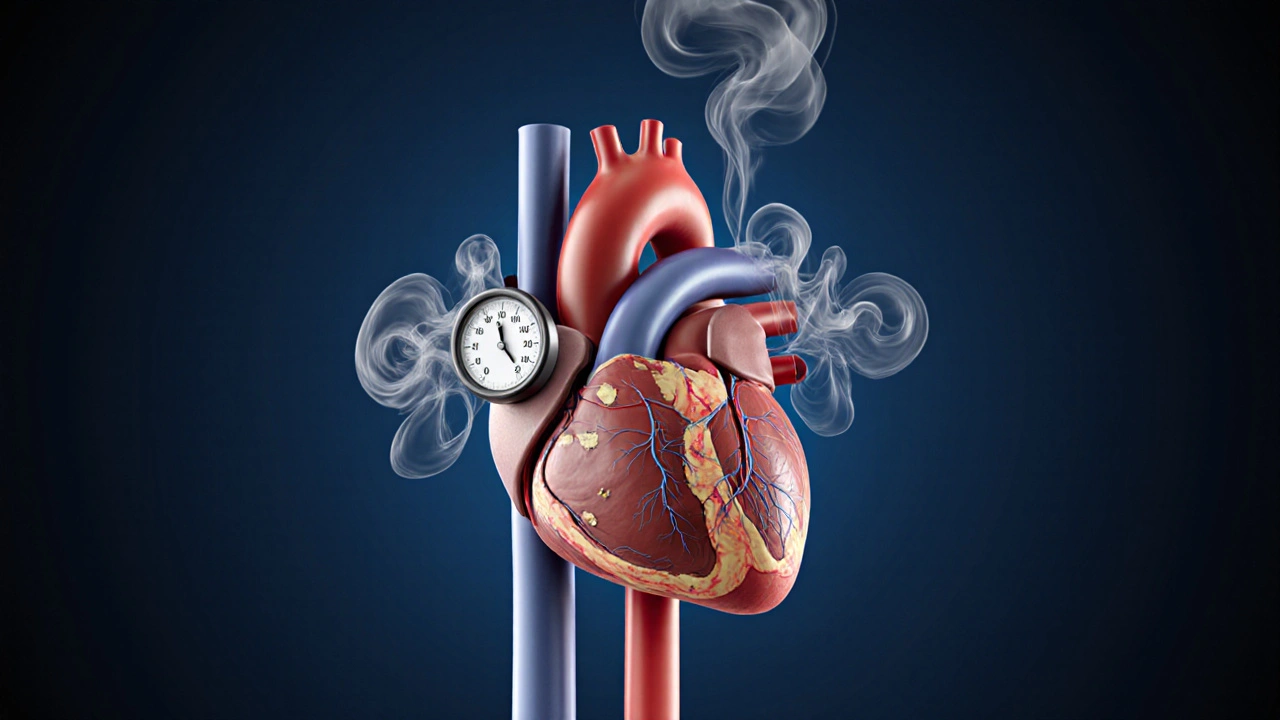
Why does quit smoking matter for someone with heart failure? First, nicotine spikes heart rate and raises blood pressure, which forces an already weakened heart to work harder. This extra strain accelerates fluid buildup and worsens shortness of breath. Second, the carbon monoxide in cigarette smoke reduces oxygen delivery to tissues, making the heart pump even more blood to meet basic needs. In short, smoking fuels a vicious cycle: nicotine addiction drives heart disease, and heart disease makes quitting feel harder. Breaking that cycle by quitting smoking directly reduces the workload on the heart, lowers blood pressure, and improves oxygen levels—all key factors in managing congestive heart failure.
Practical Steps to Stop Smoking When You Have Heart Failure
Step one is to get a clear medical picture. Talk to your cardiologist about how tobacco use is affecting your specific condition. A doctor can order tests that show how much your heart is stressed and suggest safe medications such as nicotine‑replacement therapy or prescription varenicline. Step two is to choose a cessation plan that fits your lifestyle. Some patients swear by group counseling, while others prefer a mobile app that tracks cravings and offers instant tips. The best plans combine behavioral support—like setting a quit date and identifying triggers—with pharmacologic help when needed.
Third, lean on your support network. Family, friends, and even online communities can provide encouragement when cravings hit. Sharing your quit date with loved ones creates accountability and lets them offer distractions—like a walk or a cup of herbal tea—when withdrawal symptoms appear. Fourth, manage stress without lighting up. Techniques such as deep‑breathing, gentle yoga, or even simple stretching can lower cortisol levels, which in turn reduces the urge to smoke. Remember, stress is a common trigger for both heart failure flare‑ups and smoking relapses, so tackling it on two fronts pays double dividends.
Finally, track your progress. Keep a journal of daily heart‑related symptoms—like swelling, fatigue, or weight changes—and compare them to days when you didn’t smoke. Many ex‑smokers report noticeable improvements within a few weeks: reduced coughing, easier breathing, and lower blood pressure readings. Seeing these numbers move in the right direction reinforces the decision to stay smoke‑free and gives your doctor concrete data to adjust heart‑failure medication if needed.
The link between quitting and better heart outcomes isn’t just theory; it’s backed by data. A 2022 study of 1,200 patients with congestive heart failure found that those who stopped smoking had a 30% lower risk of hospitalization over two years compared to those who continued. Another trial showed that nicotine‑replacement patches helped 45% of heart‑failure patients stay smoke‑free for at least six months, and those patients also reported higher quality‑of‑life scores.
So, what can you expect after you quit? Within 20 minutes, blood pressure begins to drop. After 12 hours, carbon monoxide levels fall, improving oxygen transport. In a few weeks, circulation improves, making it easier for your heart to pump blood. Over months, lung function recovers, reducing shortness of breath—a common symptom of heart failure. All these changes create a healthier environment for your heart to recover, slow disease progression, and possibly extend your lifespan.
Above all, remember that quitting smoking is a journey, not a single event. If you slip, don’t view it as failure; treat it as feedback on what triggers need more attention. Each quit attempt builds resilience, and many patients succeed after multiple tries. Your heart benefits from every day you stay smoke‑free, even if the path isn’t perfectly straight.
Below you’ll find a curated set of articles that dive deeper into the science, share personal stories, and offer step‑by‑step guides to help you quit smoking while managing congestive heart failure. Explore the resources, pick the strategies that fit your life, and take the next confident step toward a healthier heart.
How Smoking Affects Congestive Heart Failure & How to Quit
Learn how smoking worsens congestive heart failure, the health benefits of quitting, and a step‑by‑step quit plan with medications, counseling, and cardiac rehab support.
Health and WellnessLatest Posts
Tags
- online pharmacy
- medication safety
- generic drugs
- medication
- dietary supplement
- side effects
- online pharmacy UK
- drug interactions
- mental health
- impact
- online pharmacies
- statin side effects
- dosage
- adverse drug reactions
- generic vs brand
- pediatric antibiotics
- antibiotic side effects
- FDA drug safety
- skin health
- health




