Morphine and Liver Impairment: What You Need to Know About Dosing and Risks
When your liver, the organ responsible for breaking down most medications in your body. Also known as the body's main detox center, it plays a critical role in how drugs like morphine are processed. isn't functioning well, even standard doses of morphine can build up to dangerous levels. Morphine is mostly broken down by the liver into metabolites — some helpful, some harmful. If your liver is damaged from alcohol, hepatitis, fatty liver disease, or other conditions, it can't do this job properly. That means morphine sticks around longer, increasing the risk of overdose, extreme drowsiness, or breathing problems — even if you're taking it exactly as prescribed.
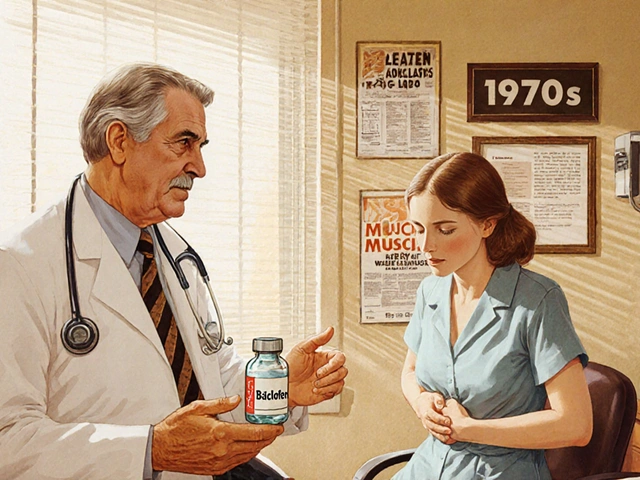
This isn't just about dose size. People with liver impairment, a condition where the liver can't perform its normal filtering and metabolic tasks often need lower doses, longer gaps between doses, or even alternative pain meds. Doctors don't always adjust automatically — many assume morphine is "safe" because it's been used for decades. But research shows that patients with moderate to severe liver disease have up to three times higher blood levels of morphine compared to healthy people. That’s why monitoring isn't optional. Signs like confusion, extreme fatigue, slow breathing, or unexplained nausea aren't just side effects — they could be early warnings of toxicity.
It's not just morphine. Other opioids, pain medications that act on the central nervous system and are metabolized by the liver like codeine, oxycodone, and hydrocodone face similar issues. But morphine is one of the most common, especially in chronic pain or end-of-life care. The problem gets worse if you're also taking other drugs that stress the liver — antibiotics, antidepressants, or even herbal supplements. Your liver doesn't care if something is "natural" or "prescribed." If it's processed there, it competes for space.
What you can do? Talk to your doctor before starting or changing any pain medication. Ask: "Is my liver okay for this?" and "Should my dose be adjusted?" Bring a list of everything you take — even over-the-counter pills. Simple blood tests like ALT, AST, and bilirubin can show liver function quickly. If your liver is impaired, switching to a drug that doesn't rely on liver metabolism — like hydromorphone or fentanyl — might be safer. But that decision needs to be made with care. You're not being overly cautious if you ask. You're being smart.
The posts below cover real-world cases and science-backed advice on how medications behave when organs like the liver are under stress. You'll find details on drug interactions, metabolic pathways, and how to spot trouble before it becomes an emergency — all written plainly, without jargon. No fluff. Just what you need to stay safe.

Opioids and Liver Disease: How Impaired Metabolism Increases Risk of Toxicity
Opioids can become dangerous in liver disease due to impaired metabolism, leading to toxic buildup. Learn how morphine, oxycodone, and other opioids behave in liver impairment-and what safer alternatives exist.
MedicationsLatest Posts
Tags
- online pharmacy
- medication safety
- generic drugs
- medication
- dietary supplement
- side effects
- online pharmacy UK
- drug interactions
- mental health
- impact
- online pharmacies
- statin side effects
- dosage
- adverse drug reactions
- generic vs brand
- pediatric antibiotics
- antibiotic side effects
- FDA drug safety
- skin health
- health