Understanding Lung Inflammation and Its Connection to Air Travel
As someone who loves to travel and explore new destinations, I often find myself boarding a plane and embarking on a new adventure. However, I recently began to wonder about the potential impact of air travel on our health, particularly with regards to lung inflammation. After conducting thorough research, I have discovered some interesting findings, which I would like to share with you in this article.
How Cabin Pressure Affects Our Lungs
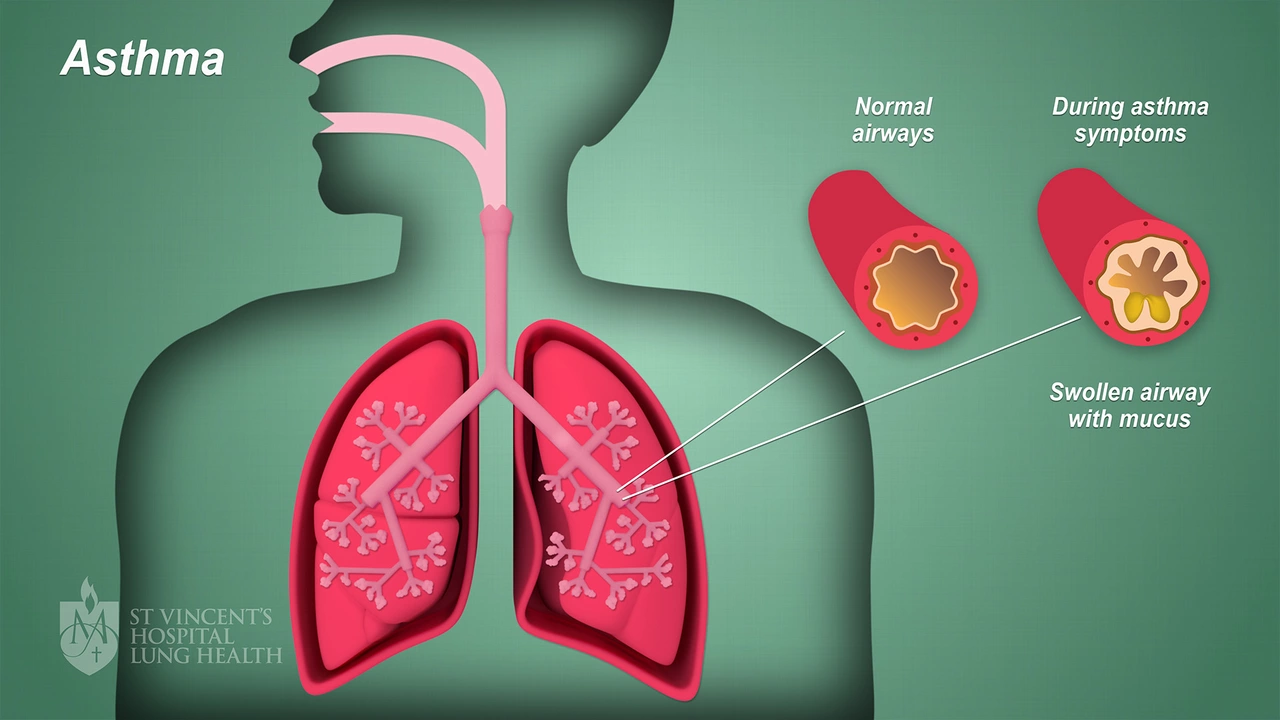
When we travel by air, we are exposed to a different environment than we are on the ground. The cabin pressure on an airplane is usually set to mimic the atmospheric pressure at an altitude of around 6,000 to 8,000 feet. This lower pressure can affect the amount of oxygen available for our bodies to absorb, potentially leading to a condition called hypoxia. Hypoxia can cause inflammation in the lungs and other respiratory issues, especially for those with pre-existing lung conditions such as asthma or chronic obstructive pulmonary disease (COPD).
Air Quality in the Aircraft Cabin
The quality of the air we breathe while flying is another factor that can impact our lung health. Air in the cabin is a mix of fresh air from outside and recirculated air from within the cabin. This air is filtered through High-Efficiency Particulate Air (HEPA) filters, which are designed to remove more than 99% of airborne particles, including bacteria, viruses, and allergens. However, these filters are not perfect, and some contaminants can still make their way into the cabin, potentially causing inflammation in the lungs of sensitive individuals.
Exposure to Secondhand Smoke and E-Cigarette Vapor
Although smoking is prohibited on most commercial flights, exposure to secondhand smoke and e-cigarette vapor can still occur in airports, especially in designated smoking areas. Secondhand smoke is a known irritant for the lungs, contributing to inflammation and potentially exacerbating existing lung conditions. Similarly, e-cigarette vapor has been found to cause inflammation in the lungs and can even harm lung cells, as demonstrated in some studies.
Long-Haul Flights and Deep Vein Thrombosis
Long-haul flights, typically those lasting more than four hours, can increase the risk of developing deep vein thrombosis (DVT). DVT occurs when a blood clot forms in a deep vein, usually in the legs, and can potentially travel to the lungs, causing a life-threatening condition called pulmonary embolism. Immobility during long flights can lead to blood pooling in the legs, promoting clot formation. While DVT is not a direct cause of lung inflammation, the potential complications associated with it can significantly impact lung health.
Reducing the Risk of Lung Inflammation During Air Travel
There are several steps we can take to minimize the risk of lung inflammation while traveling. First, it is essential to stay well-hydrated, as dehydration can contribute to inflammation. Drinking plenty of water and avoiding excessive alcohol or caffeine consumption can help maintain proper hydration levels. Additionally, practicing deep breathing exercises and moving around the cabin when possible can improve circulation and reduce the risk of DVT. Lastly, if you have a pre-existing lung condition, ensure that you have all necessary medications and equipment readily available during your flight, and consult with your healthcare provider before traveling.
Conclusion: Balancing the Benefits and Risks of Air Travel
While air travel offers us the opportunity to explore new places and cultures, it is essential to be aware of the potential risks to our lung health. By understanding the factors that contribute to lung inflammation and taking the necessary precautions, we can enjoy our travels while minimizing the impact on our respiratory systems. So, the next time you board a plane, remember these tips and enjoy a healthier and more pleasant flight experience.






Kyah Chan
6 May 2023The exposition exhibits several methodological deficiencies that merit scrutiny. The reliance on cabin pressure approximations neglects individual physiological variability, particularly among subjects with latent respiratory pathology. Moreover, the citation of HEPA filtration efficacy lacks quantification of filter degradation over successive flight cycles. The assertion that low‑level hypoxia precipitates inflammation is oversimplified, given the compensatory mechanisms of erythropoietic adaptation. Consequently, the conclusions drawn appear premature without longitudinal cohort data.
Ira Andani Agustianingrum
6 May 2023Staying hydrated and moving around really helps, keep it up!
James Higdon
6 May 2023It is incumbent upon travelers to uphold personal responsibility for their respiratory wellbeing, especially when indulging in habits that exacerbate airway irritation. The indiscriminate presence of e‑cigarette vapor in proximity to non‑users imposes an unjustifiable risk, tantamount to passive assault on pulmonary health. One must therefore eschew environments where such pollutants persist and demand stricter enforcement of smoke‑free policies. Ethical travel demands pre‑flight consultation with healthcare professionals for those with pre‑existing conditions, ensuring that preventive measures are not merely advisory but obligatory.
Wanda Smith
7 May 2023Consider, for a moment, the possibility that commercial aviation entities deliberately understate the potency of airborne contaminants to preserve market confidence, thereby masking a coordinated agenda that prioritizes profit over public health.
Bridget Jonesberg
7 May 2023One cannot discuss the ontological ramifications of airborne exposure without first acknowledging the intricate tapestry of immunological cascades that unfold within the alveolar milieu during ascent. The diminution of ambient pressure initiates a subtle hypobaric stimulus, compelling pulmonary capillaries to undergo endothelial shear stress, which, in turn, modulates cytokine release patterns. This cascade is further complicated by the presence of ultrafine particulate matter that, despite the nominal efficiency of HEPA filtration, may infiltrate the respiratory tract via micro‑leakages and recirculation pathways. The resultant oxidative stress incites a state of low‑grade inflammation that, while clinically silent, predisposes susceptible individuals to exacerbations of underlying asthma or COPD. Moreover, the hygroscopic nature of cabin air induces mucosal dehydration, thereby impairing mucociliary clearance and facilitating pathogen adherence. It is a tragic irony that the very devices designed to safeguard passengers – pressurization systems and air recirculation units – become inadvertent conduits for physiological perturbation. When we examine the longitudinal data, we observe a non‑negligible incidence of post‑flight respiratory complaints, a phenomenon that correlates with flight duration and frequency, suggesting a dose‑response relationship. The physiological stressors are compounded by behavioral variables: alcohol consumption, sedentary posture, and the occasional allure of electronic nicotine delivery systems, each contributing to a synergistic burden on the lung parenchyma. In light of these complexities, it becomes incumbent upon clinicians to counsel travelers not merely on hydration and ambulation, but on proactive pulmonary hygiene, including pre‑emptive bronchodilator use where appropriate. Finally, the onus rests upon regulatory bodies to enforce stricter air quality standards, perhaps mandating continuous real‑time monitoring of cabin particulate concentrations, thereby transforming opaque safety metrics into transparent, actionable data for the discerning voyager.