Lung inflammation: causes, signs, and what helps
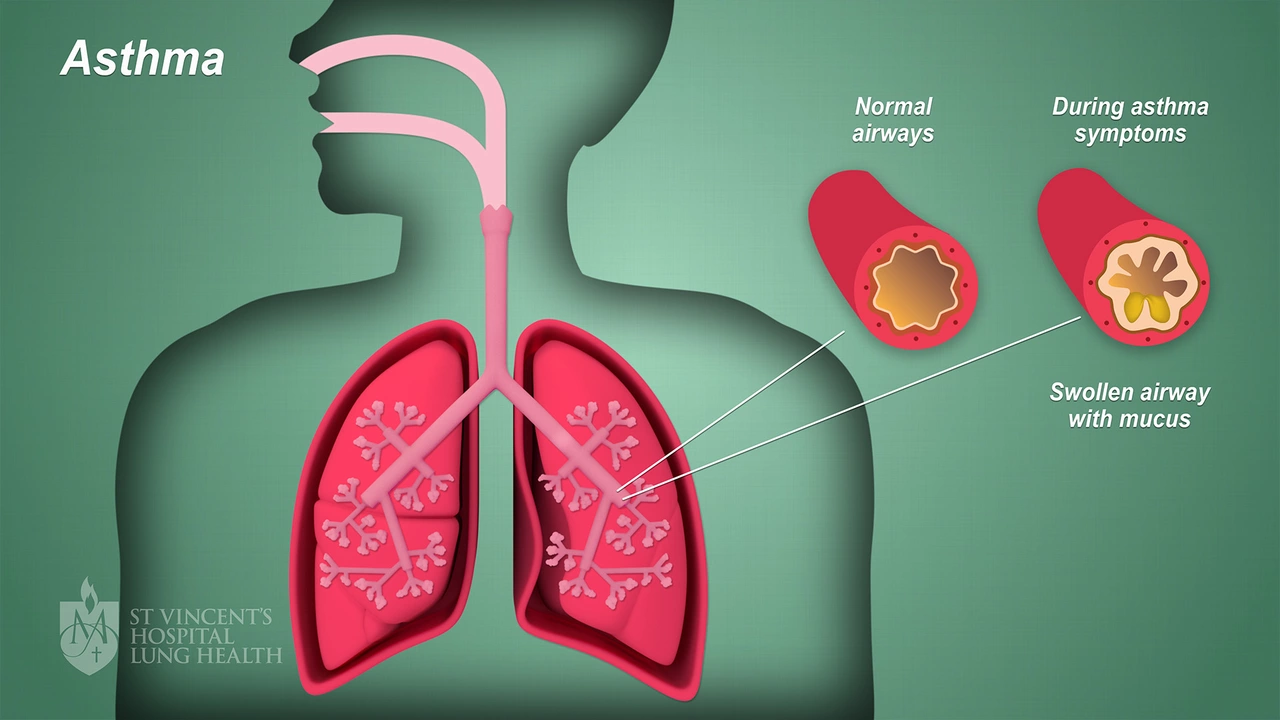
Lung inflammation happens when airways or air sacs get irritated or infected. You might feel cough, chest tightness, faster breathing, or fever. Causes range from viral infections (like the flu or COVID), bacterial infections (pneumonia), to irritants such as smoke, chemicals, or allergic reactions. Chronic conditions like asthma and COPD also cause ongoing inflammation. Knowing the likely cause steers treatment.
How do doctors figure it out? They listen to your lungs, ask about symptoms and exposures, and often use tests. A chest X‑ray shows areas of infection or fluid. Blood tests and sputum cultures can point to bacterial causes. Sometimes doctors use CT scans or bronchoscopy for tricky cases. If a viral cause is suspected, rapid flu or COVID tests may be used.
When you need medical care now
Get urgent help if you have trouble breathing, bluish lips, high fever, confusion, or chest pain that won’t stop. Shortness of breath that limits daily activities, fast breathing, or if existing conditions (like heart disease) worsen, are also red flags. Young children, older adults, and people with weak immune systems should be seen sooner rather than later—what starts mild can worsen fast.
How lung inflammation is treated
Treatment depends on the cause. For bacterial infections, antibiotics are used. For viral infections, treatment is mainly supportive—rest, fluids, and sometimes antiviral drugs when appropriate. Inhaled steroids or oral steroids reduce airway swelling in asthma or severe flare-ups. Bronchodilators open tight airways to ease breathing. Hospital care may include oxygen, IV fluids, and breathing support for severe cases.
Want practical things you can do at home? Use a humidifier or take steamy showers to loosen mucus. Stay hydrated, rest, and avoid smoke or air pollutants. Over‑the‑counter fever reducers help with comfort. If mucus is thick, warm saline gargles and breathing exercises can help clear it. Don’t use someone else’s inhaler or antibiotics—get a proper diagnosis first.
Preventing lung inflammation matters and it’s doable. Get your yearly flu shot and follow recommendations for pneumococcal vaccine if you’re at risk. Quit smoking and avoid secondhand smoke. Wear masks in dusty or polluted places, and wash hands often to cut infection risk. Manage chronic conditions like asthma with your prescribed inhalers and regular follow‑ups.
Not sure if you can treat this at home? Call your clinic or use telehealth to get quick advice. If you have a prescription history listed or need help finding reliable medicines online, check trusted pharmacies and confirm prescriptions are required. Early care often means simpler treatment and faster recovery.
How long will lung inflammation last? It depends: mild viral inflammation often improves in a week or two, bacterial cases improve within days of starting antibiotics, and chronic inflammation (from asthma or COPD) can last months unless properly treated. Follow your treatment plan, keep follow-ups, and tell your doctor if symptoms return after finishing meds. Small changes—like air filters and getting vaccines—cut flare-ups over time. If in doubt, seek care early to avoid bigger problems now.
The Impact of Air Travel on Lung Inflammation
I recently came across some fascinating research on the impact of air travel on lung inflammation. It turns out that spending long hours in the pressurized environment of an airplane can cause our lungs to be more susceptible to inflammation. This is due to factors such as reduced air quality, low humidity, and the presence of airborne pathogens. As a frequent traveler, this information has definitely caught my attention and made me rethink how I can better protect my lungs during flights. I'll be sure to look into ways to minimize these risks and share my findings with all of you in a future blog post!
Health and WellnessLatest Posts
Tags
- online pharmacy
- medication safety
- generic drugs
- medication
- dietary supplement
- side effects
- online pharmacy UK
- drug interactions
- mental health
- impact
- online pharmacies
- statin side effects
- dosage
- generic vs brand
- pediatric antibiotics
- antibiotic side effects
- skin health
- health
- pain relief
- dietary supplements




