Heart Failure Smoking Risk
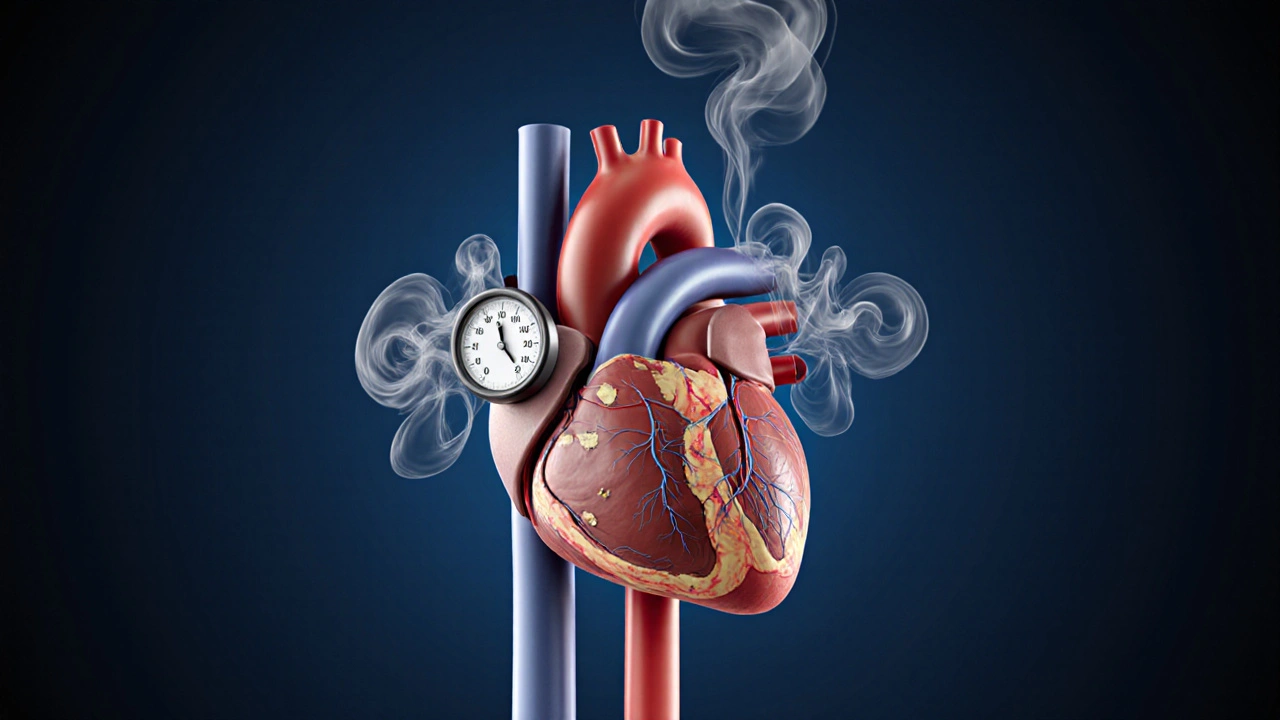
When talking about Heart Failure Smoking Risk, the added danger that tobacco use brings to people already battling heart failure. Also known as smoking and heart failure risk, it dramatically raises mortality and hospital readmission rates. Understanding this threat starts with recognizing the role of Smoking Cessation, the set of tools and programs that help a person stop using tobacco. Equally critical is Congestive Heart Failure, a condition where the heart cannot pump blood efficiently, leading to fluid buildup and fatigue. When tobacco fumes enter the bloodstream, they tighten blood vessels, raise blood pressure, and accelerate the wear and tear on an already weakened heart. The combination creates a perfect storm: higher oxygen demand, reduced oxygen delivery, and a greater chance of arrhythmias. That's why heart failure smoking risk is a top concern for cardiologists, nurses, and patients alike. Adding to the mix, Beta‑Blockers, medications that slow the heart rate and lower blood pressure, are often prescribed to manage heart failure symptoms. Smokers may need adjusted doses because nicotine spikes heart rate and can blunt the drug’s effect, so monitoring is essential.
Key Factors and Practical Steps
First, quit smoking. The data are crystal clear: stopping tobacco use lowers the risk of heart‑related death by up to 40% within five years. Programs that combine counseling, nicotine‑replacement therapy, and mobile‑app support produce the highest success rates. A simple step‑by‑step plan—identify triggers, replace the habit with a healthier activity, and lean on friends or a quit‑line—makes the journey doable. Second, manage fluid intake and sodium levels. Excess salt forces the heart to work harder, and smokers already have increased vascular resistance. Third, stick to medication regimens. For patients on Toprol XL, a common beta‑blocker (metoprolol) used in heart failure therapy, doctors may recommend a titration schedule that accounts for nicotine’s temporary blood‑pressure spikes. Fourth, adopt heart‑friendly lifestyle habits: regular low‑impact exercise, a diet rich in fruits, vegetables, and omega‑3 fatty acids, and consistent sleep patterns. Each of these actions directly counters the harmful cascade started by smoking—lowering inflammation, improving endothelial function, and stabilizing heart rhythm.
Below you’ll find a curated set of articles that dive deeper into these topics. From a detailed look at how smoking worsens congestive heart failure to proven quit‑smoking strategies and medication comparisons, the collection gives you actionable insight and real‑world tips. Use this resource to map out your next steps, whether you’re a patient seeking clearer guidance or a caregiver planning support. Let’s explore the specifics and arm yourself with the knowledge to reduce risk and improve quality of life.
How Smoking Affects Congestive Heart Failure & How to Quit
Learn how smoking worsens congestive heart failure, the health benefits of quitting, and a step‑by‑step quit plan with medications, counseling, and cardiac rehab support.
Health and WellnessLatest Posts
Tags
- online pharmacy
- medication safety
- generic drugs
- medication
- dietary supplement
- side effects
- online pharmacy UK
- drug interactions
- mental health
- impact
- online pharmacies
- statin side effects
- dosage
- adverse drug reactions
- generic vs brand
- pediatric antibiotics
- antibiotic side effects
- FDA drug safety
- skin health
- health



