When a pill leaves the factory, its job isn’t done. It still has to last-sometimes for years-without losing strength, changing color, or turning harmful. That’s where stability testing comes in. It’s not just paperwork or a box-ticking exercise. It’s the backbone of patient safety in pharmaceuticals. Every tablet, injection, or inhaler you take has been tracked, measured, and monitored under real-world conditions for months or even years before it ever reaches your medicine cabinet.
Why Stability Testing Isn’t Optional
Imagine a cancer drug that loses half its potency after six months. Or an antibiotic that breaks down into toxic chemicals when stored in a warm bathroom. These aren’t hypotheticals. In 2021, nearly 1 in 6 drug recalls in the U.S. were tied to stability failures-potency loss, unexpected degradation, or contamination. The FDA doesn’t just ask for stability data; it demands it. Without it, no new drug gets approved.
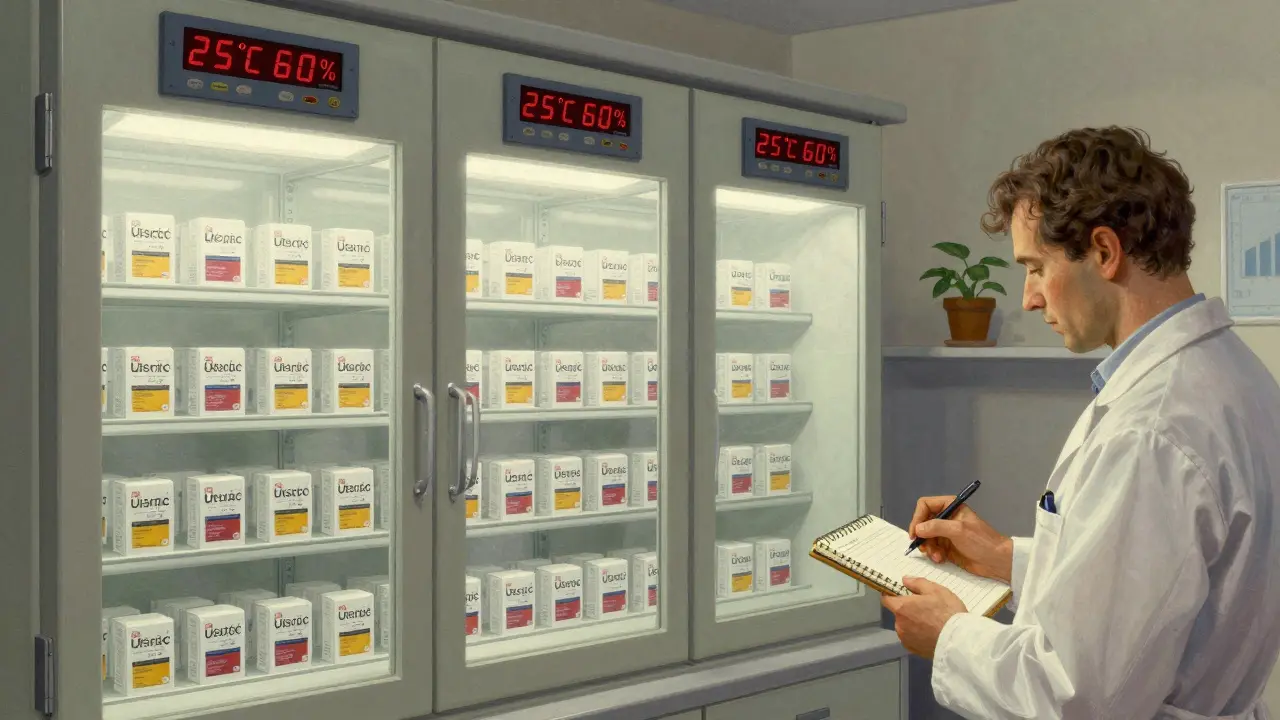
The science behind this is simple but rigorous. Manufacturers place packaged drugs into climate-controlled chambers that mimic real-life conditions: 25°C and 60% humidity for most markets, or 30°C and 65% humidity for hotter regions like Southeast Asia or the Middle East. These aren’t random settings-they’re based on decades of global research and formalized in the ICH Q1A(R2) guidelines from 2003. Testing happens at 0, 3, 6, 12, 24, and 36 months. At each interval, samples are pulled and analyzed for changes in appearance, chemical composition, dissolution rate, and microbial growth.
This isn’t about guessing. It’s about proving. Every test method must be validated. Every result must be traceable. And every deviation triggers an investigation. If a batch shows a 5% drop in active ingredient after 18 months, that’s not a minor issue-it’s a red flag. The drug might still be safe, but if it’s no longer effective, it’s a failure. And patients rely on it working exactly as promised.
How It’s Done: The Technical Side
Stability testing doesn’t just check if a pill still looks the same. It digs deep. Here’s what’s measured:
- Assay: Is the active ingredient still at 95-105% of the labeled amount?
- Degradation products: Are any new chemicals forming? Even trace amounts of impurities can be dangerous.
- Dissolution: Does the tablet still break down in the body the same way?
- Physical properties: Color, texture, odor, pH, and even how easily it crumbles.
- Microbial limits: Especially for sterile products like injections-no mold, no bacteria.
These aren’t simple tests. They require high-precision tools like HPLC (High-Performance Liquid Chromatography), GC-MS (Gas Chromatography-Mass Spectrometry), and validated analytical methods that can detect changes smaller than 0.1%. One misstep in calibration, and the whole study is invalid.
And then there’s the environment. Stability chambers aren’t regular fridges. They’re precision instruments, monitored 24/7. Temperature and humidity must stay within ±2°C and ±5% RH. If a power outage causes a 3-hour spike to 32°C, that’s an excursion. It’s logged, investigated, and may invalidate data from that shelf. One company in Australia lost 8 months of data-and $2.3 million in delayed market entry-because of a humidity glitch. That’s not rare. In fact, 68% of pharma quality teams say chamber maintenance is their biggest headache.
Accelerated Testing: A Shortcut with Limits
Waiting three years to find out if a drug lasts five years isn’t practical. So companies use accelerated testing: 40°C and 75% humidity for six months. It’s meant to simulate years of aging in a fraction of the time.
But here’s the catch: it’s a prediction, not proof. A 2021 study in the Journal of Pharmaceutical Sciences showed that accelerated data correctly predicted shelf life in 83% of cases-but failed in the rest. For complex drugs like biologics (protein-based treatments for autoimmune diseases or cancer), accelerated testing often misses critical degradation pathways. That’s why real-time data is still the gold standard. No algorithm can replace real-world time.
Some companies try to cut corners. They rely on mean kinetic temperature (MKT) calculations-common in food or cosmetics-but those aren’t accepted by the FDA or EMA for drugs. Why? Because drugs aren’t bread. One molecule out of place can turn a lifesaver into a danger.
Costs, Challenges, and the Human Factor
Stability testing isn’t cheap. A single product study can cost between $50,000 and $150,000. For a company with 20 products, that’s over $1 million a year. Add in chamber qualification ($8,500 per chamber every quarter), method validation (3-6 months per test), and data management, and you’re looking at $500,000 to $2 million annually just for stability.
That’s why 72% of pharma companies outsource to CROs like SGS, Eurofins, or Charles River. But outsourcing doesn’t mean less responsibility. The manufacturer still owns the data. If the CRO makes a mistake, the FDA comes after the brand, not the lab.
And the paperwork? It’s massive. Each stability protocol must include at least 15 required elements: sampling plans, acceptance criteria, storage conditions, test methods. The final report needs 20+ data points per product. Paper files are outdated. Most companies now use electronic systems, but validating those systems takes 6-9 months. One company saved $120,000 a year by reducing sample sizes using ICH Q12 principles-but only after 18 months of internal training and process overhaul.
Real Wins, Real Failures
Stability testing has prevented disasters. In 2022, SGS found a hidden chemical reaction between a new biologic drug and its glass vial. The drug was degrading into a toxic compound. The launch was halted. The vial was redesigned. An estimated $500 million in losses were avoided.
On the flip side, a 2021 FDA warning letter cited a manufacturer that ignored out-of-spec results for a cancer drug. They didn’t investigate. They didn’t report. The drug got approved. Later, patients reported reduced effectiveness. The company faced a 14-month delay in approval, fines, and reputational damage.
Dr. Jennifer Orme of Pfizer says robust stability programs cut post-market recalls by 31% since 2015. The International Pharmaceutical Aerosol Consortium found stability testing blocked 47 unsafe products from reaching patients between 2020 and 2022. That’s not just compliance-it’s protection.

The Future: Faster, Smarter, Risk-Based
Change is coming. In February 2023, the ICH finalized Q13, new guidelines for stability testing in continuous manufacturing-a shift away from batch-based testing. The FDA is pushing for real-time monitoring during production. And AI is starting to help.
By 2027, machine learning models could predict degradation patterns with 80% accuracy, cutting testing time by 30-40%. Instead of waiting 36 months, companies might run 6 months of data through a trained algorithm to forecast 5-year stability. That’s not science fiction-it’s already happening in pilot programs at top pharma firms.
But don’t expect the old system to disappear. Even with AI, regulators will still demand real-time data for new, complex, or high-risk products. The trend isn’t to eliminate testing-it’s to make it smarter. Risk-based approaches, like those outlined in ICH Q12, let companies reduce testing for well-understood, stable drugs. For example, a simple aspirin tablet might need less scrutiny than a gene therapy product.
What’s clear: stability testing isn’t going away. As personalized medicines, biologics, and complex drug delivery systems grow, the need for precise, long-term monitoring will only increase. The future isn’t fewer tests-it’s better data, faster insights, and smarter decisions.
What You Need to Know
If you’re a patient: trust that your medication has been tested for years before it got to you. The expiration date isn’t arbitrary-it’s science-backed.
If you work in pharma: stability testing isn’t a cost center. It’s your shield against recalls, delays, and worse-harm to patients. Don’t cut corners. Don’t ignore outliers. Document everything.
If you’re a startup: don’t underestimate this. Budget for it early. Hire or contract experts. A stability failure can kill a product before it even launches.
Stability testing is the quiet guardian of pharmaceutical quality. It doesn’t make headlines. But when it works, it keeps millions safe. When it fails, people get hurt. That’s why it’s not optional. It’s essential.
What is the purpose of stability testing in pharmaceuticals?
Stability testing determines how a drug’s quality changes over time under specific environmental conditions like temperature and humidity. It’s used to set expiration dates, define storage requirements, and ensure the product remains safe, effective, and pure throughout its shelf life. Without this data, regulators won’t approve the drug for sale.
How long does stability testing take?
Real-time stability testing typically runs for 24 to 36 months, with samples tested at 0, 3, 6, 12, 18, 24, and 36 months. Accelerated testing (40°C/75% RH) lasts 6 months and is used to predict long-term behavior, but it’s not a substitute for real-time data. For new drugs, the full study must be completed before regulatory approval.
What are ICH guidelines for stability testing?
The ICH Q1A(R2) guideline sets global standards for stability testing. It defines standard conditions: 25°C/60% RH for temperate climates and 30°C/65% RH for hot/humid regions. Accelerated conditions are 40°C/75% RH for 6 months. It also requires stability-indicating methods, specific testing intervals, and statistical analysis for shelf-life determination. These are mandatory for FDA and EMA submissions.
Can stability testing be outsourced?
Yes, over 70% of pharmaceutical companies outsource stability testing to contract research organizations (CROs) like SGS, Eurofins, or Charles River Laboratories. However, the drug manufacturer remains legally responsible for the data’s accuracy and compliance. Outsourcing can reduce costs but requires strict oversight and validation of the CRO’s processes.
What happens if a stability test fails?
A failed stability test triggers an out-of-specification (OOS) investigation. The company must determine if the failure is due to a manufacturing flaw, storage issue, or testing error. If the drug is no longer safe or effective, the batch may be rejected, recalls may be initiated, or regulatory submissions may be delayed. In severe cases, the FDA can issue warning letters or block product approval entirely.
How is stability testing changing with new technology?
New technologies like AI and machine learning are being used to predict degradation patterns from limited data, potentially reducing testing timelines by 30-40% by 2027. ICH Q13 now supports real-time monitoring in continuous manufacturing. Quality by Design (QbD) and ICH Q12 allow risk-based testing, reducing sample sizes for well-understood products. But core requirements-real-time data, validated methods, and regulatory compliance-remain unchanged.







Christina Widodo
12 January 2026So many people think expiration dates are just there to make us buy more medicine, but this post broke it down like I’ve never seen before. I had no idea the chambers are monitored to within ±2°C and ±5% RH. That’s insane precision. And the part about the Australian company losing $2.3M because of a humidity glitch? Mind blown.
Prachi Chauhan
13 January 2026stability testing is like waiting for a plant to grow but you’re watching a pill age. it’s not magic, it’s math and patience. if the pill changes, the person using it might not get better. simple as that. no need for fancy words.
Katherine Carlock
14 January 2026I work in healthcare admin and I used to roll my eyes at all the paperwork… until I saw a recall notice from a drug that failed stability. People got sick. Not because of bad intent, but because someone skipped a step. This isn’t bureaucracy-it’s the last line of defense. Thank you for writing this.
Sona Chandra
14 January 2026WHY DO WE STILL LET BIG PHARMA GET AWAY WITH THIS? THEY OUTSOURCE TO CROs AND THEN BLAME THE LABS! THEY’RE MAKING BILLIONS WHILE PATIENTS PAY THE PRICE FOR CUTTING CORNERS! THIS IS A SCAM AND YOU KNOW IT!
Jennifer Phelps
16 January 2026the 0.1% detection threshold is wild. one molecule out of place and boom toxic. and yet we still use accelerated testing like it’s gospel. i get why but still… feels like gambling with lives
beth cordell
17 January 2026👏👏👏 THIS IS WHY I TRUST MY MEDS. NO ONE TALKS ABOUT THIS BUT IT’S THE REASON I’M STILL ALIVE. THANK YOU FOR DOING THE WORK SO WE DON’T HAVE TO WORRY. 🙏💊
Lauren Warner
18 January 2026Let’s be real. 72% outsource because they don’t want to pay for the infrastructure. The FDA doesn’t audit every CRO. The data is only as good as the person who entered it. And no one checks the metadata. This whole system is built on trust, not verification.
Lelia Battle
19 January 2026It’s fascinating how stability testing mirrors the human condition-time reveals what we try to hide. A pill, like a person, may look unchanged on the surface, but internal shifts can be catastrophic. The rigor here isn’t just scientific-it’s ethical.
Konika Choudhury
19 January 2026India makes 40% of the world's generic drugs and we do stability testing better than anyone. USA and EU still rely on old methods. We have cheaper labs and smarter people. Stop doubting us. We save lives too.
Darryl Perry
20 January 2026Costs $50K-$150K per product. That’s why generics are cheaper. But if the testing is done right, why does the price still go up? Hypocrisy.
Windie Wilson
22 January 2026So let me get this straight… we spend years testing a pill so it doesn’t turn into poison… but we still let people store it in a hot bathroom? 🤦♀️ I’m not mad, I’m just disappointed.
Daniel Pate
22 January 2026The real win here isn’t the tech or the AI. It’s the cultural shift: from ‘get it approved’ to ‘make sure it lasts’. That’s a quiet revolution. The scientists doing this work don’t get awards. They just keep the world from breaking.
Amanda Eichstaedt
24 January 2026I used to think expiration dates were a scam. Then my grandma took a heart med past its date and had a bad reaction. It wasn’t the drug’s fault-it was ours for not understanding how fragile these molecules are. This post? It’s a love letter to the unseen workers who keep us alive.
Jose Mecanico
26 January 2026Thanks for sharing this. I’m in supply chain and I never realized how much goes into one pill. Now I see why delays happen. It’s not laziness-it’s science taking its time. Respect.