Every year, around 476,000 people in the U.S. get Lyme disease. That’s not the number you hear on the news-it’s the real number, estimated from insurance records. Official reports only show about 30,000 cases. Why the gap? Because many people aren’t diagnosed until it’s too late. And by then, the damage is already done.
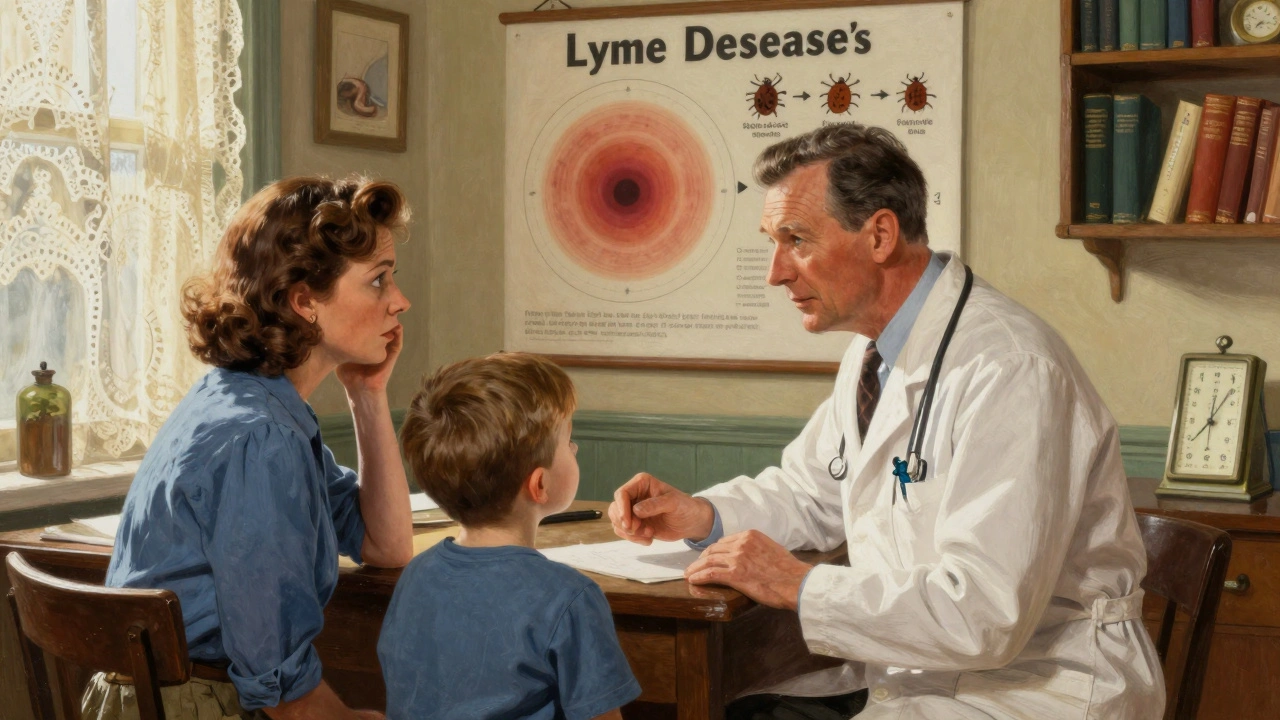
How Lyme Disease Starts
Lyme disease isn’t caught from air, water, or touch. It comes from a tiny tick-smaller than a poppy seed. These are blacklegged ticks, or Ixodes scapularis, found mostly in the Northeast, Mid-Atlantic, and Upper Midwest. In California, it’s the Western blacklegged tick. They don’t jump or fly. They wait on grass or bushes, latch on when you brush past, and start feeding.The bacteria that cause Lyme, Borrelia burgdorferi, live in the tick’s gut. But they don’t jump into you right away. It takes time. Most experts agree: the tick needs to be attached for at least 24 hours. Some studies say it can start as early as 15 hours. Either way, if you find a tick and remove it within a day, your risk drops by 95%.
That’s why checking yourself after being outdoors matters. Showering within two hours helps wash off unattached ticks. A full-body tick check-behind the ears, under the arms, in the groin, behind the knees-isn’t optional. It’s your first line of defense.
The Three Stages of Lyme Disease
Lyme disease doesn’t hit all at once. It unfolds in stages, each with its own timeline and symptoms.Stage 1: Early Localized (1-28 days after bite)
This is the easiest stage to catch-and the most treatable. About 70-80% of people develop a rash called erythema migrans. It looks like a bull’s-eye: a red circle that expands outward, sometimes clearing in the middle. It’s not itchy or painful, so people often ignore it. But it’s the clearest sign of Lyme.
Other early signs? Fever (45% of cases), fatigue (70%), headache (61%), muscle aches, swollen lymph nodes. These feel like the flu. That’s why so many people get misdiagnosed. If you’ve been in a tick area and feel sick, don’t wait for the rash. Get checked.
Stage 2: Early Disseminated (weeks to months after bite)
If the infection isn’t treated, the bacteria spread. Now you’re in Stage 2. Symptoms get worse and more confusing.
You might get multiple rashes. Nerve problems show up: facial paralysis (Bell’s palsy), tingling in hands or feet. Heart issues can develop-Lyme carditis. That’s when the bacteria interfere with your heart’s electrical signals. It can cause dizziness, shortness of breath, or skipped heartbeats. About 4-10% of untreated cases get this.
Stage 2 is when lab tests become more useful. Antibodies start showing up in blood. But even then, they’re not perfect. Early tests miss up to 35% of cases because your body hasn’t made enough antibodies yet.
Stage 3: Late Disseminated (months to years after bite)
This is what happens when Lyme goes untreated for too long. It’s rare, but devastating.
Chronic joint pain-especially in the knees-is common. Up to 60% of untreated patients develop arthritis that comes and goes. Nerve damage can lead to numbness, shooting pains, or brain fog. Memory problems, trouble focusing, and mood changes are reported by many. Some patients describe it as “Lyme brain.”
At this point, treatment gets harder. Antibiotics still help, but recovery takes longer. And for some, symptoms linger even after treatment.
Treatment: What Works and What Doesn’t
Here’s the good news: if caught early, Lyme disease is almost always cured.
For Stage 1, doctors prescribe 10-21 days of oral antibiotics. Doxycycline is standard for adults. Kids and pregnant people get amoxicillin or cefuroxime. These drugs kill the bacteria before they spread. Most people feel better in days. Symptoms usually disappear completely within weeks.
Stage 2 and 3? That’s where things change. If nerves or the heart are involved, you’ll need IV antibiotics-usually ceftriaxone-for 14-28 days. Hospital stays aren’t always needed; some people get IV treatment at home.
But here’s the controversy: what about people who still feel sick after treatment?
Dr. Allen Steere, the scientist who first identified Lyme disease, says the bull’s-eye rash is diagnosis enough. No test needed. The Infectious Diseases Society of America (IDSA) says prolonged antibiotics don’t help and can be dangerous. They call persistent symptoms “Post-Treatment Lyme Disease Syndrome” (PTLDS), not ongoing infection.
PTLDS affects 10-20% of treated patients. Fatigue, joint pain, brain fog-these can last over six months. Johns Hopkins research shows it’s real, but not caused by live bacteria. It’s likely an autoimmune reaction or lingering inflammation.
Some doctors, especially those in ILADS, disagree. They treat with longer courses of antibiotics. Twenty-eight U.S. states have laws protecting them from punishment for doing so. But there’s no solid proof it helps. And long-term antibiotics carry risks: C. diff infections, antibiotic resistance, liver damage.
One thing’s clear: the sooner you start treatment, the better your odds. A CDC study found 87% of patients treated within 30 days of symptoms fully recovered within three months.
Testing: What You Can and Can’t Rely On
Doctors use two-tiered blood tests: ELISA first, then Western blot if the first is positive. But they’re flawed.
In Stage 1, they only catch 29-40% of cases. Why? Your body hasn’t made enough antibodies yet. By Stage 2 and 3, sensitivity jumps to 87%. But false positives happen too-especially if you’ve had other infections like syphilis or mononucleosis.
That’s why diagnosis should never rely on labs alone. If you have the rash? You have Lyme. No test needed.
There’s new hope. In March 2023, the FDA approved the MiQLick test, which detects Lyme bacteria DNA in urine. It’s 92% accurate in early disease. That’s a big leap. But it’s not widely available yet.
And a vaccine? It’s coming. Valneva and Pfizer are testing VLA15, a vaccine targeting multiple Lyme strains. Phase 2 results showed 70-96% effectiveness. Human trials are underway. If approved, it could be the first Lyme vaccine in decades.
Prevention: What Actually Works
There’s no magic spray or bracelet. But there are proven steps.
- Wear long pants tucked into socks when hiking or gardening in tick areas.
- Use EPA-approved repellents with DEET, picaridin, or permethrin (on clothes, not skin).
- Check yourself, your kids, and your pets every time you come inside.
- Remove ticks with fine-tipped tweezers. Grasp close to the skin. Pull straight up. Don’t twist. Don’t use matches, nail polish, or Vaseline.
- Save the tick in a sealed bag with the date. If you get sick later, it helps doctors.
For high-risk areas, a single 200mg dose of doxycycline within 72 hours of a tick bite can prevent infection-if the tick was attached for over 36 hours and is identified as a blacklegged tick. Talk to your doctor before you go hiking. Ask if prophylaxis is right for you.

What to Do If You Think You Have Lyme
If you’ve been bitten and feel unwell:
- Don’t wait for the rash. See a doctor immediately.
- Describe your outdoor exposure and symptoms honestly.
- Ask about the possibility of Lyme-even if the test is negative.
- If your doctor dismisses you, seek a second opinion. Many patients see 3-7 doctors before getting diagnosed.
- Document everything: dates, symptoms, treatments.
Delay costs you time, energy, and health. The average time to diagnosis? 1.8 years. That’s 22 months of pain, confusion, and wasted visits. You don’t have to wait that long.
What’s Next for Lyme Disease?
Climate change is making things worse. Ticks are moving north. In Canada, their habitat expanded by 50% between 2000 and 2020. More people are being exposed. By 2050, Lyme cases could double.
Research is accelerating. mRNA vaccines are in development. Better diagnostic tools are being tested. And more doctors are learning to recognize the early signs.
But until then, your best defense is awareness. Know the risks. Know the signs. Act fast.
Can you get Lyme disease from a dog?
No, you can’t catch Lyme disease directly from a dog. But dogs can carry infected ticks into your home. If your dog has ticks, check yourself and your family. Use tick preventatives on pets-it reduces your risk too.
Is Lyme disease contagious between people?
No. Lyme disease is not spread through kissing, sex, blood transfusions, or breastfeeding. There’s no evidence it passes from mother to baby during pregnancy, though untreated infection may pose risks. The only way you get it is through an infected tick bite.
Do all ticks carry Lyme disease?
No. Only blacklegged ticks (Ixodes species) carry the bacteria, and not all of them are infected. In high-risk areas, 20-50% of ticks may carry Lyme. In low-risk areas, it’s far less. Location and tick species matter more than just seeing a tick.
Can you get Lyme disease more than once?
Yes. Getting Lyme once doesn’t make you immune. You can be bitten again by another infected tick. That’s why prevention never stops-even after recovery.
Why do some people still feel sick after treatment?
About 10-20% of people have lingering symptoms like fatigue, joint pain, or brain fog after antibiotics. This is called Post-Treatment Lyme Disease Syndrome (PTLDS). It’s not an active infection. Researchers believe it’s due to immune system changes or tissue damage from the original infection. It usually improves over time, but can last months or longer. There’s no proven cure yet, but physical therapy, pacing, and sleep support can help.
If you live in or visit the Northeast, Mid-Atlantic, or Upper Midwest, treat every tick bite seriously. You don’t need to live in fear-but you do need to be informed. The clock starts ticking the moment a tick latches on. Don’t wait for symptoms. Act fast. Your body will thank you.





David Brooks
7 December 2025Just got back from a hike in Vermont and did my full tick check-found one behind my knee. Removed it with tweezers in 10 seconds. No panic, just relief. This post saved my ass. Thanks for the clear info. I’m telling everyone I know. 🙌
Sadie Nastor
8 December 2025omg i had the bullseye rash last summer and my dr said ‘probably just a bug’… i cried in the parking lot. took 4 months and 3 doctors to get diagnosed. please, if you see that rash-just go. no test needed. you’ll thank yourself later. 🌿💔
Nicholas Heer
8 December 2025They’re lying. The CDC is in bed with Big Pharma. They don’t want you to know that Lyme is a bioweapon disguised as a tick disease. They’ve been suppressing the truth since the 90s. The ‘PTLDS’ label? That’s gaslighting. IV antibiotics for 6 months? That’s the REAL cure. And they’re silencing doctors who dare to help. #LymeCoverUp
Stacy here
10 December 2025Let’s be real-this isn’t just about ticks. It’s about how our healthcare system fails people who don’t fit the textbook. I’ve seen friends go from hiking enthusiasts to bedridden for years because no one listened. The science is messy, yes. But the suffering? That’s real. And we need to stop pretending it’s ‘all in your head’ just because the test is negative. #ListenToPatients
Kyle Flores
12 December 2025My mom had Lyme in the 90s and was told she was ‘just anxious.’ She spent 3 years in pain before someone finally listened. I keep this post saved. I showed it to my sister after she got bit last week. She went to the doctor the same day. No rash, but fever. Got antibiotics. She’s fine now. Prevention + action = survival.
Olivia Hand
12 December 2025Wait-so if I get bit by a tick in Oregon, I’m not at risk? But I read that Western blacklegged ticks are spreading. And what about deer ticks in the South? Are we just ignoring the new hotspots? This post feels like it’s stuck in 2010. The map’s changing. The science needs to catch up.
Louis Llaine
13 December 2025So… you’re telling me I have to check my ass after every walk in the park? And carry tweezers? And save ticks like they’re tiny evidence? Next you’ll tell me to wear a hazmat suit to the grocery store. I’ll take my chances. At least I don’t have to Google ‘is this a tick or a speck of dirt’ every time I sweat.
Nancy Carlsen
14 December 2025My niece got Lyme at 7. She couldn’t walk for months. We’re so lucky she got diagnosed early. Now she’s back to ballet. This post? It’s a gift. Please share it with every parent, teacher, coach, camp counselor. Kids don’t always say ‘I feel weird.’ We have to be the ones who notice. 🌻
Ted Rosenwasser
15 December 2025Let’s not romanticize this. The ‘bullseye rash’ appears in less than half the cases. The rest? Non-specific flu-like symptoms. You’re encouraging mass overdiagnosis. The MiQLick test? Still experimental. VLA15? Phase 2 isn’t Phase 3. Don’t confuse hope with science. This isn’t a movie. It’s medicine. And medicine requires evidence, not emotion.
Helen Maples
16 December 2025Stop saying ‘it’s just PTLDS.’ That’s not a diagnosis-it’s a dismissal. If your body is still in pain after antibiotics, you’re not ‘imagining it.’ You’re not lazy. You’re not crazy. You’re fighting inflammation. And you deserve better than ‘take ibuprofen and rest.’ We need research funding. We need doctors trained. We need validation. Not platitudes.
Ashley Farmer
18 December 2025Thank you for mentioning the tick removal technique. So many people twist or burn them. I’ve had 3 friends get infections from bad removal. Just grab close, pull straight up, clean the area. It’s simple. But nobody teaches it. This info could save someone’s knee, their heart, their brain.
Jennifer Anderson
18 December 2025i had lyme 2x. both times i missed the rash. second time i thought i had mono. took 5 months. now i check my dog every day. he’s my little tick detector. also-don’t wear white socks. wear dark. ticks are easier to spot. and yes, i save the tick in a ziplock. weird? maybe. saved my life? definitely.
Kurt Russell
18 December 2025YOU CAN DO THIS. If you’ve been misdiagnosed, you’re not broken. You’re not alone. I was told I had chronic fatigue for 2 years. Turns out? Lyme. Got treated. Got my energy back. Took time. Took patience. Took a doctor who listened. You’re stronger than the doubt. Keep going. The clock’s ticking-but so are you. 💪
Ryan Sullivan
19 December 2025The entire narrative around Lyme is a perfect storm of medical negligence, media sensationalism, and patient desperation. The IDSA guidelines are evidence-based. ILADS is a cult. The ‘long-term antibiotics’ movement is a dangerous placebo economy. This post, while well-intentioned, dangerously blurs the line between science and speculation. You’re not helping-you’re enabling.
David Brooks
21 December 2025Replying to @TedRosenwasser: I get that you want ‘evidence.’ But what’s the evidence for ignoring someone in pain because their test came back negative? My sister’s heart skipped beats for months. Her test was negative. She got IV antibiotics anyway. She’s fine now. Evidence isn’t just in labs-it’s in lives.