Medication Safety Risk Calculator
Your Medication Safety Risk Assessment
Your Risk Assessment Results
Based on your responses, we've calculated your risk of medication side effects. This tool incorporates data from the British Heart Foundation, AHRQ, and other medical sources as discussed in the article.
Key risk factors affecting your score
When you pick up a new prescription, the doctor looks at your current symptoms, but how often do they dig into your full medical past? Your medical history can dramatically shape how you react to a drug, turning a routine treatment into a painful side‑effect nightmare. This article breaks down the key historical factors that crank up the odds of medication side effects and shows you practical ways to stay one step ahead.
Adverse drug reactions are unwanted, harmful effects that occur at normal drug doses - they’re not rare accidents. In fact, studies from the British Heart Foundation and the Agency for Healthcare Research and Quality (AHRQ) show that millions of adults experience at least one ADR each year, and a big chunk of those could be avoided by reviewing a patient’s history.Why Your Past Health Matters for Drug Safety
Think of your body as a busy highway. Medications travel along routes that can be blocked, rerouted, or slowed by existing conditions. Chronic illnesses, surgeries, or previous drug allergies leave footprints that affect absorption, distribution, metabolism, and excretion - the four pillars of pharmacokinetics. Ignoring these footprints is like sending a delivery truck through a road closed for construction.
Polypharmacy: The Biggest Red Flag
Taking many drugs at once isn’t just a numbers game; it’s a potent risk multiplier. The British Heart Foundation’s 2023 analysis found that patients on five to nine medicines were 100% more likely to suffer an ADR compared with those on fewer than five, and those on ten or more faced a 300% increase. Each extra pill adds roughly a 7‑10% bump in risk, according to AHRQ’s 2023 meta‑analysis.
Why does this happen? Multiple drugs compete for the same metabolic enzymes, push the kidneys harder, and raise the chance of unintended drug‑drug interactions. Even over‑the‑counter painkillers can tip the balance.
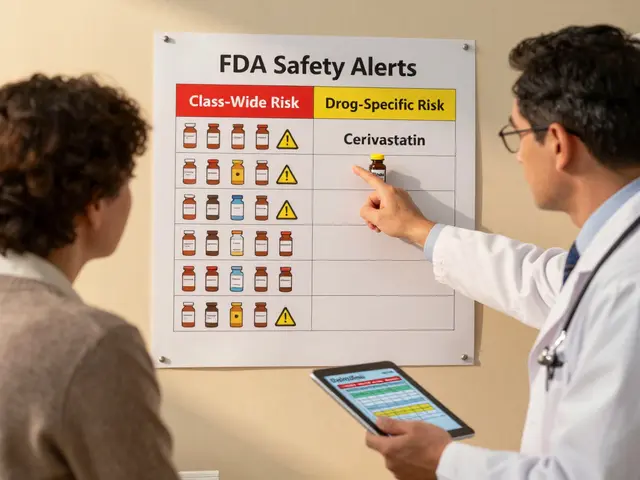
Genetics and Liver Metabolism - The Role of CYP450 Enzymes
Not everyone processes drugs the same way. Variations in the CYP450 family of liver enzymes can boost drug levels by 30‑500%, turning a standard dose into a toxic one. For instance, a CYP2D6 poor metabolizer may experience severe side effects from codeine because the body can’t convert it efficiently into its active form.
Pharmacogenomic tests, like the FDA‑cleared YouScript platform, screen for 27 gene‑drug interactions and have been shown to cut ADRs by about 34% in patients with relevant variants. Yet, as of Q2 2024, fewer than 6% of U.S. health systems use such testing routinely.
Kidney and Liver Disease: How They Change Drug Handling
Chronic kidney disease (CKD) reduces renal clearance by 50‑75%, meaning drugs that rely on the kidneys linger longer and can reach toxic concentrations. The American Medical Association reported that 40% of commonly prescribed medicines need dose adjustments for CKD patients, but electronic health records only flag this correctly 35% of the time.
Hepatic impairment is another silent danger. Liver disease impairs metabolism, especially for drugs cleared by CYP enzymes. The AMA notes that 25% of medications require changes for patients with liver dysfunction.
Both conditions demand careful dose tailoring - a simple misstep can sky‑rocket the risk of nausea, bleeding, or even organ failure.
Age and Gender - The Overlooked Factors
Older adults, especially those over 65, experience 3‑5 times more ADRs than younger people, according to the American Geriatrics Society. Age‑related declines in liver mass, blood flow, and renal function all play a part.
Gender matters, too. The British Heart Foundation found older women suffer ADRs at least 50% more often than men, likely because historic clinical trials under‑represented women (only 22% in cardiovascular drug trials from 2010‑2020). This leads to dosing guidelines that don’t fully account for sex‑specific pharmacokinetics.
Past Drug Reactions and Cross‑Reactivity
A documented allergy to one drug class raises the odds of a reaction to a similar class by 30‑40%. For example, patients with a penicillin allergy have an eight‑fold higher chance of reacting to certain cephalosporins. The 2009 BMC Family Practice study highlighted that historical drug‑interaction patterns account for 28% of serious ADRs.
Electronic health records often miss these nuances. A 2022 Johns Hopkins audit showed only about a third of records flagged prior allergies in a way that would trigger alerts during e‑prescribing.
How to Reduce Your Risk - Practical Steps
- Maintain an up‑to‑date medication list, including over‑the‑counter drugs and supplements.
- Ask your clinician about any past drug reactions, even those that seemed mild.
- Discuss genetic testing if you have a family history of unusual drug responses.
- Ensure renal and liver function tests are current before starting new medicines.
- Request a structured medication review, especially if you’re on five or more drugs. Deprescribing programs have lowered ADRs by roughly 22%.
- Report any new symptoms promptly - side effects can mimic disease signs.
Quick Reference: Historical Risk Factors & Relative Increase
| Factor | Typical Impact | Evidence Source |
|---|---|---|
| Polypharmacy (5‑9 meds) | 100% higher risk | British Heart Foundation 2023 |
| Polypharmacy (10+ meds) | 300% higher risk | British Heart Foundation 2023 |
| Age > 65 | 3‑5× more ADRs | American Geriatrics Society 2022 |
| Chronic kidney disease | 40% of meds need dose change | American Medical Association 2023 |
| Hepatic impairment | 25% of meds need adjustment | American Medical Association 2023 |
| Prior drug allergy (same class) | 30‑40% higher cross‑reactivity | BMC Family Practice 2009 |
| CYP450 polymorphism | 30‑500% increase in drug levels | Merck Manual 2024 |
| Female gender (older) | ≥50% more ADRs than men | British Heart Foundation 2023 |
What to Expect From Your Healthcare Team
Good clinicians ask three simple questions before signing a prescription: (1) What’s your current medication list? (2) Do you have any known drug allergies or past reactions? (3) How are your kidneys and liver doing? If any answer raises a flag, they should order labs, adjust the dose, or consider an alternative.
If you feel your history isn’t being considered, speak up. A clear, concise summary of your past conditions - especially CKD, liver disease, or previous ADRs - can prompt a safer prescribing decision.
How many medications count as polypharmacy?
Clinicians usually define polypharmacy as the regular use of five or more prescription or over‑the‑counter drugs. Risks rise sharply after the third medication and climb dramatically after five.
Can genetic testing really prevent side effects?
Yes. Pharmacogenomic panels identify variants in enzymes like CYP2C19 or CYP2D6 that affect drug metabolism. Patients with actionable results can have doses lowered, switched, or avoided altogether, cutting ADR rates by roughly one‑third in studied groups.
What should I do if I develop a new symptom after starting a drug?
Report it right away. Keep a log of the symptom’s timing, severity, and any other meds or foods you’ve taken. Your doctor can then decide if it’s a side effect, a drug‑drug interaction, or something unrelated.
Are over‑the‑counter drugs part of the risk assessment?
Absolutely. Ibuprofen, antihistamines, and supplements can interact with prescription drugs. Bring every pill, even vitamins, to your medication review.
How often should I get my medication list reviewed?
If you’re on five or more drugs, aim for an annual comprehensive review. For high‑risk groups - seniors, people with CKD, liver disease, or a history of ADRs - a review every six months is wise.





Lennox Anoff
25 October 2025It is a travesty that modern medicine continues to parade the illusion of omniscience while ignoring the very foundations of patient history. The cavalier attitude of prescribers, who treat a prescription like a one‑size‑fits‑all solution, betrays a profound disrespect for individual lived experience. When a clinician fails to probe the labyrinth of past illnesses, surgeries, and drug reactions, they are essentially gambling with lives.
Consider the cascade of consequences when polypharmacy is introduced without a meticulous audit; each additional pill is not merely a number, but a potential catalyst for catastrophe. Yet the system rewards volume over vigilance, urging doctors to fill charts rather than to listen.
It is a moral imperative to demand that every medication list be scrutinized like a legal contract, with clauses for renal function, hepatic capacity, and genetic predispositions. The data from the British Heart Foundation and AHRQ are not abstract statistics-they are a clarion call for ethical stewardship.
We must champion the patient’s right to a comprehensive review, lest we become complicit in preventable adverse drug reactions. In the grand theatre of healthcare, the audience should never be the unwitting victim of a plot twist they could have foreseen.
Charlie Stillwell
26 October 2025Wow, another fluff piece pretending to be science 🙄. Let’s cut the crap – the pharma machine knows your DNA better than you do, and they’re not telling you because it hurts their bottom line 😡. All that talk about "pharmacogenomics" is just a marketing gimmick to dump more expensive tests on patients. Your kidneys? Your liver? Yeah, they’re just side‑effects of a system designed to keep you on pills forever. Wake up, people! 🚨💊
Ken Dany Poquiz Bocanegra
27 October 2025Great overview! Keeping an updated medication list is simple yet powerful. It lets you and your clinician spot potential interactions before they become a problem. Even a brief note about past drug reactions can save weeks of discomfort. Stay proactive – it’s the best defense against unwanted side effects.
Buddy Bryan
29 October 2025If you’re on multiple prescriptions, you need a systematic approach. First, write down every medication, including vitamins and OTC drugs. Then, cross‑reference each with known CYP450 pathways – a quick online tool can flag major interactions. Next, schedule a lab check for renal and hepatic panels before any new drug is added. Finally, ask your pharmacist to run a medication therapy management review; they have the expertise to catch hidden risks that doctors often overlook. Ignoring these steps is a recipe for avoidable adverse reactions.
Jonah O
29 October 2025i dunt think they want u to know how deep the con is they are hiding the real test data they only want us to think its random errors but the pattern is there the whole system is riggged it us not a coincidence look at the 6% usage stat they dont want u to chec k you know they get paid for the missed opport u nities
Aaron Kuan
30 October 2025Side effects suck.
Nathan Comstock
31 October 2025Patriots, hear this! Our great nation cannot afford a populace crippled by careless prescriptions. The very blood that built this country runs through every vein, and we must guard it against the pharmaceutical leviathan that seeks profit over health. Demand thorough reviews, know your kidneys, demand genetic testing if needed – these are not luxuries, they are rights for every American who values liberty and life!
Amber Lintner
31 October 2025Oh please, the drama queen’s anthem again. You think a patriotic rant will magically fix your medication list? Spoiler: it won’t. What you need is humility, not hollow slogans. Maybe try listening to actual guidelines instead of shouting about “rights” while ignoring the simple steps already laid out.
the sagar
1 November 2025Listen, the globalists hide the fact that most drugs are engineered to fail your body unless you stay dependent. They don’t want you to get genetic testing because it would expose their profit scheme. The system is a trap – keep your eyes open.
Grace Silver
1 November 2025While the concerns raised are understandable, it is essential to balance skepticism with evidence. The data supporting pharmacogenomic testing derive from rigorous trials and peer‑reviewed studies. Engaging constructively with healthcare providers and requesting transparent discussions about risks can empower patients without succumbing to unfounded conspiracy narratives.
Clinton Papenfus
2 November 2025Esteemed community members, it is with great enthusiasm that I encourage you all to adopt a holistic perspective on medication safety. By integrating cultural humility, patient education, and rigorous clinical protocols, we can foster an environment where adverse drug reactions are minimized. Let us unite in this noble endeavor and champion the health of our diverse societies.