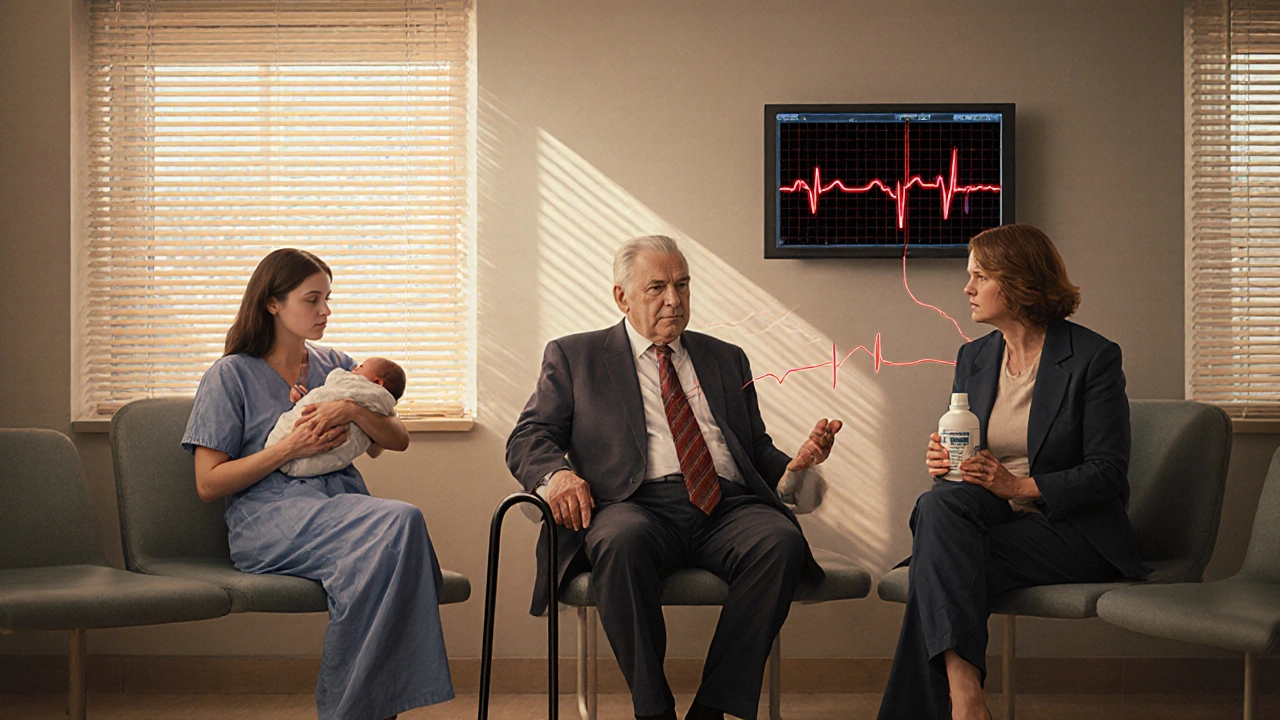
When a medication changes the way your heart beats - not in a good way - it can be life-threatening. QT prolongation is one of those silent dangers. It doesn’t cause symptoms until it’s too late. No chest pain. No dizziness at first. Just an abnormal delay in the heart’s electrical reset, visible only on an ECG. And when that delay gets too long, it can trigger torsades de pointes, a chaotic, deadly heart rhythm that can turn into cardiac arrest.
What Exactly Is QT Prolongation?
The QT interval on an ECG measures how long it takes for the heart’s lower chambers (ventricles) to recharge after each beat. This pause is critical. If it’s too short, the heart can’t fill properly. If it’s too long, the electrical system becomes unstable. That’s when torsades de pointes can start - a spiral of erratic heartbeats that can kill within minutes. This isn’t rare. Since the 1950s, doctors have known certain drugs cause this. In 2013, the FDA found that 22% of tested drugs - 46 out of 205 - could prolong the QT interval. By 2025, crediblemeds.org listed over 220 medications with known or possible links to this risk. Most of these aren’t heart drugs. They’re things you might take for a stomach bug, depression, or infection.How Do Drugs Cause This?
The main culprit is the hERG potassium channel. This tiny protein in heart cells helps the heart reset after beating. Many drugs accidentally block it. When that happens, the heart takes longer to recharge. The longer the delay, the higher the risk. The most dangerous QT prolongation happens when the corrected QT interval (QTc) hits 500 milliseconds or more - or when it jumps more than 60 ms from your normal baseline. That’s not a guess. That’s backed by data from thousands of cases. And women are at higher risk. About 70% of documented torsades cases happen in women, especially after childbirth or in older age.Medications That Carry the Highest Risk
Not all QT-prolonging drugs are created equal. Some are high-risk, others low. Here’s who’s on the list:- Class Ia and III antiarrhythmics: Quinidine, procainamide, sotalol, dofetilide. These are designed to treat arrhythmias - but they can cause them too. Quinidine causes torsades in about 6% of patients. Sotalol, even at normal doses, raises risk by 2-5%.
- Antipsychotics: Haloperidol, ziprasidone, thioridazine. Ziprasidone has a black box warning from the FDA for sudden cardiac death. Even at standard doses, these can push QTc over 500 ms in vulnerable people.
- Antibiotics: Erythromycin, clarithromycin, azithromycin. Erythromycin can lengthen QTc by 15-25 ms. Combine it with a CYP3A4 inhibitor (like fluconazole or grapefruit juice), and the risk spikes.
- Antidepressants: Citalopram and escitalopram. The FDA limited citalopram to 40 mg daily (20 mg for those over 60) because of clear dose-dependent QT effects. Even at 20 mg, some patients hit the danger zone.
- Antiemetics: Ondansetron (Zofran). It’s widely used for nausea. But in 68% of documented torsades cases from 2015-2019, ondansetron was involved - often with another QT-prolonging drug.
- Methadone: Used for pain and addiction. Doses over 100 mg/day are especially risky. Many patients on long-term methadone have QTc >500 ms without knowing it.
- Antifungals: Fluconazole, ketoconazole. Fluconazole isn’t as bad as some, but at high doses (400 mg/day), it can add 10-20 ms to QTc.
- Oncology drugs: Vandetanib, nilotinib, sunitinib. Over 40% of new cancer drugs approved since 2015 carry QT warnings. These are often used in frail, elderly patients with multiple other risk factors.

It’s Not Just the Drug - It’s the Combination
One QT-prolonging drug? Risk is low. Two or three? Risk jumps dramatically. A 2017 study showed that combining haloperidol with ondansetron raised torsades risk more than either drug alone. That’s not a fluke. In real-world cases, 68% of torsades incidents involved multiple drugs. Even common over-the-counter meds can add up. Antihistamines like diphenhydramine, some cough syrups with dextromethorphan, and even herbal supplements like St. John’s wort can interfere with drug metabolism and raise levels of QT-prolonging drugs. Electrolyte imbalances make it worse. Low potassium, low magnesium, low calcium - all of these make the heart more sensitive to drug effects. A patient on a diuretic for high blood pressure who takes ondansetron for nausea? That’s a perfect storm.Who’s Most at Risk?
You might think only older people or those with heart disease are at risk. But it’s more complex:- Women: 2-3 times more likely than men to develop torsades. Hormonal differences and slower drug clearance play a role.
- Older adults: Kidneys and liver clear drugs slower. QTc naturally increases with age.
- People with heart disease: Scarred tissue, heart failure, or prior heart attack make the heart more electrically unstable.
- Those with genetic risk: About 30% of drug-induced torsades cases involve hidden mutations in the hERG gene. You might never know you’re at risk until a drug triggers it.
- People on multiple meds: The more drugs you take, the higher the chance of dangerous interactions.
What Should You Do?
If you’re prescribed a new medication - especially one on the high-risk list - here’s what matters:- Ask your doctor: “Does this drug affect my heart’s rhythm?” Don’t assume it’s safe just because it’s common.
- Get a baseline ECG: Especially if you’re over 65, female, on multiple drugs, or have heart disease. This isn’t optional for high-risk meds.
- Check your electrolytes: A simple blood test for potassium and magnesium can prevent disaster.
- Watch for warning signs: Unexplained dizziness, fainting, palpitations, or sudden fatigue. These aren’t normal. Call your doctor.
- Don’t mix drugs without checking: Use tools like crediblemeds.org or ask your pharmacist. Many hospitals now have EHR alerts - but not all do.
How Is This Being Managed Today?
The medical world is waking up. The FDA’s CiPA initiative (Comprehensive in vitro Proarrhythmia Assay) no longer just looks at QT interval. It tests drugs on multiple ion channels and uses computer models to predict real-world risk. Since 2016, 22 drugs have been dropped from development because of this. Hospitals are also improving. One 12-hospital system cut dangerous drug combinations by 58% after adding automated alerts in their electronic records. The European Society of Cardiology now recommends ECGs before starting high-risk drugs and again within 3-7 days. But gaps remain. Many primary care doctors still don’t check QTc routinely. Pharmacists report confusion over which combinations are safe. And patients? Most have no idea their antidepressant or antibiotic could be quietly stressing their heart.What’s Next?
New tools are coming. In 2024, researchers trained an AI to predict torsades risk with 89% accuracy - not just by measuring QTc, but by analyzing tiny waveform patterns invisible to the human eye. Genetic testing for hERG variants is becoming more accessible. And in 2025, new drug applications will be required to include full multi-channel safety data. Still, the biggest protection remains awareness. If you’re on any of these medications, don’t panic. But do ask questions. Know your risk. Get tested if needed. Because QT prolongation doesn’t announce itself. It waits. And when it strikes, it’s often too late.Can a single medication cause torsades de pointes?
Yes, but it’s rare at normal doses in healthy people. Most cases happen when multiple risk factors combine - like taking two QT-prolonging drugs, having low potassium, being female, or having kidney disease. Still, drugs like sotalol, quinidine, and methadone can trigger torsades even alone in vulnerable individuals.
Is QT prolongation always dangerous?
No. Mild prolongation (QTc 450-499 ms) is common and often harmless, especially in athletes or older adults. Danger starts when QTc exceeds 500 ms or increases by more than 60 ms from baseline. At that point, the risk of torsades rises sharply.
Can I take Zofran (ondansetron) if I’m on an antidepressant?
It depends. Ondansetron can prolong QTc, especially at higher doses (above 16 mg). If you’re on citalopram, escitalopram, or certain antipsychotics, combining them with ondansetron increases torsades risk significantly. Always check with your doctor or pharmacist. In many cases, alternatives like metoclopramide (with caution) or non-drug options are safer.
How often should I get an ECG if I’m on a QT-prolonging drug?
Guidelines recommend a baseline ECG before starting the drug, then a repeat within 3-7 days after starting or after any dose increase. For long-term use, especially with methadone or amiodarone, quarterly ECGs are often advised. If you develop symptoms like dizziness or fainting, get an ECG immediately.
Are there any safe alternatives to QT-prolonging drugs?
Yes, in many cases. For nausea, alternatives to ondansetron include metoclopramide (though it has its own risks) or non-drug options like ginger. For depression, sertraline or venlafaxine have lower QT risk than citalopram. For infections, azithromycin can sometimes be replaced with amoxicillin or doxycycline. Always discuss alternatives with your provider - don’t stop meds on your own.
Can I check my QT interval at home?
Not reliably. While some smartwatches claim to detect arrhythmias, they cannot accurately measure QTc. QT prolongation requires a 12-lead ECG interpreted by a trained professional. Home devices may miss subtle changes or give false reassurance. If you’re on a high-risk drug, rely on clinical ECGs, not wearables.





Sarbjit Singh
18 November 2025this is wild i had no idea my zofran could do this 😅 my grandma was on it after chemo and then got dizzy one day... turns out she was on erythromycin too. never thought to check. thanks for the heads up!
Angela J
19 November 2025they're hiding this on purpose. the pharma companies know how many people die from this and they just keep pushing the drugs. the FDA? totally bought out. i saw a whistleblower video last year-they buried 37 cases in 2022 alone. don't trust any prescription anymore.
Sameer Tawde
20 November 2025great breakdown. seriously, if you're on more than 3 meds, ask your pharmacist to run a QT interaction check. it takes 2 minutes. could save your life. #knowyourdrugs
Jeff Hakojarvi
22 November 2025i work in med-surg and see this way too often. a 72yo woman on citalopram + ondansetron + furosemide? yeah, she’s gonna have a bad day. we started doing baseline ECGs on anyone over 65 on any of these meds-cut our code blues by half. don’t wait for collapse to act.
Timothy Uchechukwu
23 November 2025why do we even need all these drugs anyway? in my village we use ginger for nausea and prayer for depression. now you tell me a pill can kill you just by sitting in your body? this is western medicine madness. they want you sick forever so you keep buying
Ancel Fortuin
24 November 2025oh so now we’re blaming the drugs? funny how no one mentions that 90% of these patients are also on 5 other meds, drink grapefruit juice, and don’t eat bananas. it’s not the drug. it’s the chaos. stop playing victim.
Bruce Bain
25 November 2025so if i take an antibiotic and a mood pill, my heart might go crazy? wow. i just thought my heart skips a beat sometimes because i drink too much coffee. guess i need to learn more.
Jonathan Gabriel
25 November 2025if the hERG channel is so fragile, why did evolution leave it vulnerable? is this just a glitch in the human design? or did we evolve to be slowly poisoned by modern chemicals? maybe torsades isn't a side effect... maybe it's a feature. a biological filter for over-medicated societies.