HIV Treatment Timeline Simulator
Simulate Your HIV Treatment Journey
Enter your diagnosis timeline to see how early treatment affects outcomes
Your Treatment Timeline
Confirmed HIV diagnosis with laboratory test
CD4 count: , Viral load:
Treatment discussion and adherence planning
Antiretroviral therapy begins immediately
Viral load recheck; early treatment leads to faster viral suppression
Your Early Treatment Advantage
Early treatment preserves your immune system and reduces transmission risk. Starting ART within 30 days of infection cuts transmission risk by more than 90%.
Quick Takeaways
- Zidovudine was the first approved antiretroviral drug and still saves lives when used early.
- Diagnosing HIV within weeks of infection improves immune recovery and reduces transmission.
- Starting combination antiretroviral therapy (ART) on the same day as diagnosis yields the best long‑term outcomes.
- Monitoring CD4 count and viral load guides treatment adjustments and prevents drug resistance.
- Side‑effects are manageable with proper counseling and supportive care.
How Zidovedine Works
When treating HIV, Zidovudine is an antiretroviral medication classified as a nucleoside reverse transcriptase inhibitor (NRTI). It mimics the natural nucleoside thymidine, gets incorporated into the viral DNA chain during reverse transcription, and then halts further elongation. This simple block stops the virus from replicating inside CD4+ T‑cells.
The drug’s half‑life is about 1 hour, so it’s usually given twice daily with food to keep plasma levels steady. Because it targets a fundamental step in the HIV life cycle, resistance can develop if the virus mutates the reverse transcriptase enzyme. That’s why zidovudine is never used alone; it’s paired with at least two other drugs from different classes.
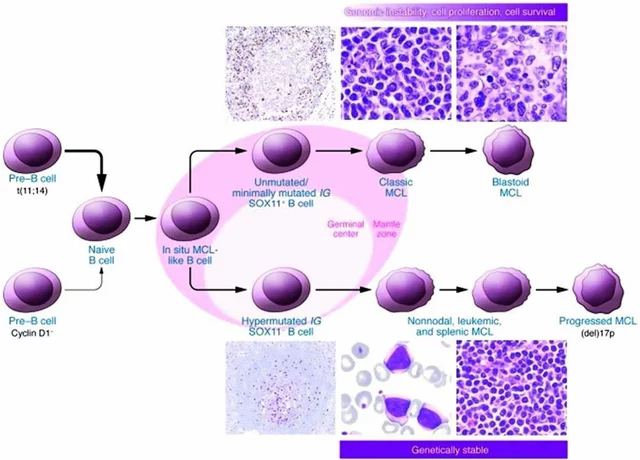
Why Early HIV Diagnosis Is a Game‑Changer
Human Immunodeficiency Virus (HIV) begins its assault the moment it enters the bloodstream. The first weeks, called acute infection, often present with flu‑like symptoms, but many people miss this window. Studies from the World Health Organization (WHO) show that starting ART within 30 days of infection cuts the risk of onward transmission by more than 90%.
Early diagnosis also preserves the CD4+ T‑cell pool. A higher CD4 count at treatment start means the immune system can rebound faster, reducing opportunistic infections and the likelihood of progressing to acquired immunodeficiency syndrome (AIDS). Moreover, the viral reservoir-cells that hide the virus-remains smaller when therapy begins promptly, a key factor in future cure research.
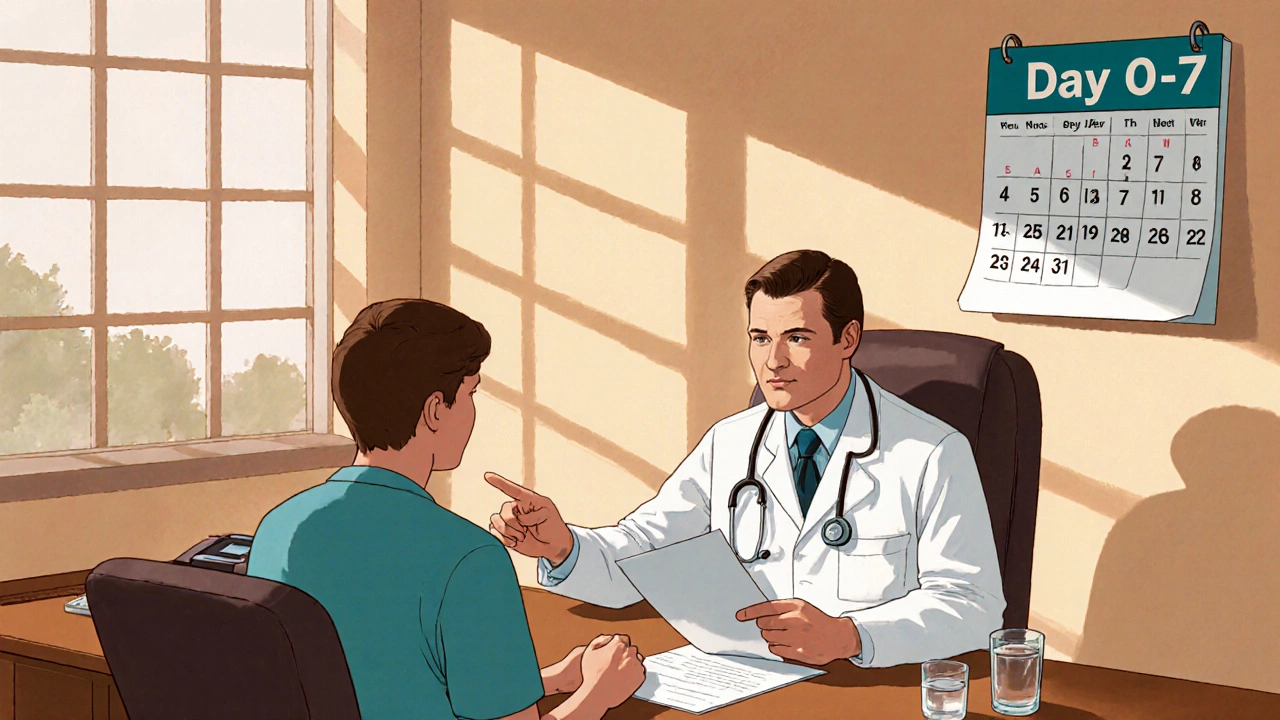
Timeline: From Positive Test to First Dose
- Day 0-7: Confirmatory testing. After an initial rapid test, a laboratory‑based HIV‑1/2 antigen/antibody combination assay confirms infection.
- Day 8-14: Baseline labs. Measure CD4 count, HIV‑1 RNA (viral load), renal and hepatic function. These values guide drug selection and dosing.
- Day 15: ART counseling. Discuss regimen options, importance of adherence, potential side‑effects, and confidentiality concerns.
- Day 16: First dose. Same‑day initiation of a three‑drug regimen-often two NRTIs (e.g., zidovudine + lamivudine) plus an integrase inhibitor-starts the viral suppression cascade.
- Weeks 2-4: Follow‑up. Repeat viral load; an undetectable result (<50 copies/mL) indicates the regimen is working.
- Months 6-12: Long‑term monitoring. CD4 recovery, resistance testing if viral load rebounds, and management of chronic side‑effects.
Skipping any step can delay suppression, increase transmission risk, and allow drug‑resistant strains to emerge.
Managing Zidovudine Side‑Effects
While zidovudine is life‑saving, it can cause anemia, neutropenia, and gastrointestinal upset. Here’s how clinicians keep patients comfortable:
- Baseline labs: A full blood count before starting identifies those at risk for anemia.
- Nutrition support: Iron‑rich foods and supplements mitigate hemoglobin drops.
- Dose adjustments: If hemoglobin falls below 8 g/dL, clinicians may reduce the dose or switch to a less‑myelotoxic NRTI.
- Co‑prescribed agents: Using growth factors like filgrastim can boost neutrophil counts when needed.
Regular monitoring-every 2-4 weeks during the first three months-catches problems early, keeping patients on track for viral suppression.
Comparing Zidovudine with Other NRTIs
| Drug | Typical Dose | Half‑Life | Common Side‑Effects | Resistance Barrier |
|---|---|---|---|---|
| Zidovudine | 300 mg PO BID | 1 h | Anemia, neutropenia, nausea | Low - single‑mutation can confer resistance |
| Lamivudine | 150 mg PO BID | 5-7 h | Headache, mild GI upset | Moderate - often used in dual‑NRTI backbones |
| Tenofovir disoproxil fumarate (TDF) | 300 mg PO QD | 17 h | Kidney toxicity, reduced bone density | High - requires multiple mutations |
| Emtricitabine | 200 mg PO QD | 10 h | Rash, mild GI symptoms | High - complimentary to tenofovir |
Choosing zidovudine today often hinges on patient‑specific factors: pregnancy (where zidovudine is safe), anemia risk, and drug‑interaction profiles. In resource‑limited settings, its low cost remains a major advantage.
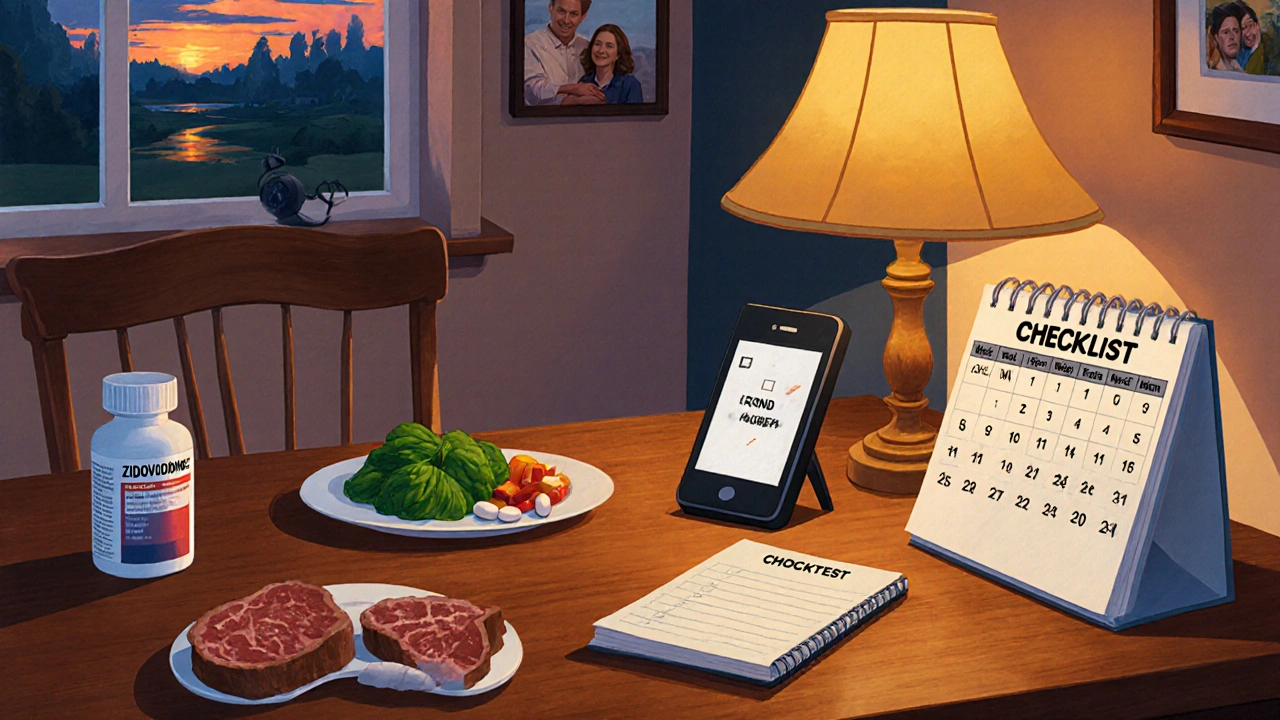
Practical Checklist for Patients Starting Zidovudine
- Bring baseline labs (CBC, renal panel, liver enzymes) to your first pharmacy visit.
- Set a daily reminder-phone alarm or pillbox-to take the dose with food.
- Watch for fatigue or shortness of breath; report any drop in energy to your clinician.
- Schedule blood tests at weeks 2, 4, and 12 to track hemoglobin and neutrophil trends.
- Maintain a healthy diet rich in iron (spinach, red meat) and B12 (eggs, dairy).
- Keep a log of side‑effects; many improve after the first month as the body adjusts.
- Never miss a dose-if you do, take it as soon as you remember unless it’s close to the next scheduled dose.
Sticking to the checklist maximizes the chance of achieving an undetectable viral load within 3-6 months.
Frequently Asked Questions
Can zidovudine be used during pregnancy?
Yes. Zidovudine has a long safety record for preventing mother‑to‑child transmission. Guidelines from the CDC recommend it as part of a combination regimen for pregnant people living with HIV.
Why is same‑day ART initiation important?
Starting treatment right after diagnosis dramatically reduces the viral set‑point, lowers transmission risk, and allows immune recovery to begin earlier. Delays of weeks can let the virus establish a larger reservoir.
What should I do if I develop anemia while on zidovudine?
Inform your clinician immediately. They may run a full blood count, adjust the dose, add iron supplementation, or switch you to another NRTI with less myelotoxicity.
How often should viral load be checked after starting treatment?
Guidelines suggest a test at 4-8 weeks, then at 6 months, and annually thereafter if the result stays undetectable.
Is zidovudine still relevant with newer drugs available?
Absolutely. In many low‑resource settings, its low cost and extensive safety data make it a cornerstone of first‑line therapy, especially for pregnant patients.
Bottom Line
Early HIV diagnosis paired with prompt initiation of a zidovudine‑based regimen can halt disease progression, protect partners, and keep communities healthier. By following the practical steps outlined above, patients and clinicians alike can turn a once‑fatal diagnosis into a manageable chronic condition.





Nicole Boyle
19 October 2025Zidovudine remains a cornerstone NRTI, especially when initiated during acute infection; the pharmacokinetics demand twice‑daily dosing with food to maintain plasma troughs. Early viral suppression curtails the establishment of the latent reservoir, a point often underscored in treatment guidelines. The CD4+ T‑cell nadir is less precipitous when therapy starts within weeks, translating to fewer opportunistic infections. Moreover, combination ART mitigates resistance pathways that monotherapy would inevitably select for. It’s a clear illustration of why diagnostics and rapid linkage to care are non‑negotiable.
Caroline Keller
26 October 2025Honestly the drama around “new drugs” is overblown, early detection and a solid AZT‑based regimen does the job just fine. Too many people think they need the latest hype while ignoring the proven benefits of something like zidovudine. It’s not about flash, it’s about consistency and adherence. Stop chasing unicorns and get tested, get treated, move on.
Jameson The Owl
1 November 2025Zidovudine, or AZT as it is colloquially known, is not merely a relic of early antiretroviral therapy; it is a pivotal component in the geopolitical chessboard of pharmaceutical control. The swift rollout of combination ART within thirty days of infection is presented as a triumph of modern medicine, yet the undercurrents suggest a calculated strategy to bind patients to lifelong dependence on proprietary drug pipelines. One must contemplate the timing of FDA approvals coinciding with corporate lobbying efforts, a pattern that repeats across therapeutic classes. The half‑life of AZT, a mere hour, necessitates bi‑daily dosing, an adherence demand that subtly enforces patient interaction with the healthcare system, thereby generating continuous revenue streams for both manufacturers and insurers. Additionally, the emphasis on viral load monitoring creates an ecosystem of diagnostic consumables that further entrench market monopolies. The sanctuary offered by early viral suppression is, in practice, a double‑edged sword: while it reduces transmission risk dramatically, it also diminishes the visibility of treatment failure, potentially masking emerging resistance mutations that could later compromise generic alternatives. The persistent recommendation to pair zidovudine with other agents underscores a deliberate avoidance of monotherapy, ostensibly to thwart resistance, yet simultaneously reinforcing poly‑pharmacy models that inflate costs. Consider the global health initiatives that tout “test‑and‑treat” as humanitarian altruism; their funding often originates from entities with vested interests in sustaining drug acquisition programs. The interplay between public health messaging and corporate profit motives is not coincidental. Early diagnosis campaigns, while beneficial on the surface, also serve as conduits for data collection, enabling longitudinal tracking of viral epidemiology that can be leveraged for market forecasting. The narrative of a “cure” hinges on a reduced viral reservoir, a concept that aligns neatly with the commercial appeal of next‑generation latency‑reversing agents, which are positioned as the inevitable successors to current regimens. In sum, zidovudine’s role extends beyond its biochemical activity; it is a linchpin in a broader strategy to institutionalize dependence on a cycle of innovation, patenting, and perpetual consumption, masquerading as patient‑centered care while perpetuating a system of economic control.
Rakhi Kasana
8 November 2025The imperative for early testing is not just a clinical recommendation, it’s a moral duty. Delaying diagnosis prolongs suffering and fuels community transmission, which contradicts the ethical principle of non‑maleficence. When patients start ART within the first month, the immune reconstitution is markedly superior, reducing the incidence of opportunistic disease. The data from WHO consistently show that same‑day initiation translates to higher rates of viral suppression at 24 weeks. In short, rapid linkage to care embodies both scientific rigor and compassionate practice.
Sarah Unrath
14 November 2025i cant stress enough how importnt it is to get tested early. the sooner u start azt + other meds the less likely u will have severe sideeffects. Also the labs need to be done as fast as possble and start treatment same day if possible
James Dean
21 November 2025Early intervention resembles a philosophical commitment to preventive stewardship; by confronting the virus before it entrenches, we preserve agency. The balance between pharmacodynamics and patient autonomy is delicate, yet achievable through clear counseling. When the viral load dips below detectability swiftly, the narrative shifts from survival to quality of life.
Monika Bozkurt
27 November 2025From a clinical standpoint, initiating zidovudine in conjunction with lamivudine and an integrase inhibitor aligns with current treatment algorithms endorsed by major health organizations. This regimen not only achieves rapid viral suppression but also minimizes the risk of resistance development. The structured follow‑up schedule-viral load reassessment at weeks 2 and 4-is essential for confirming therapeutic efficacy and adjusting therapy if needed. Moreover, patient education regarding potential hematologic side‑effects, such as transient anemia, fosters adherence and mitigates concerns. In summary, early diagnosis coupled with a well‑designed combination therapy provides the optimal pathway toward long‑term immunologic recovery.
Penny Reeves
4 December 2025The post glosses over the nuanced pharmacoeconomics of zidovudine. While it’s true that early initiation is beneficial, the simplistic narrative ignores cost‑effectiveness analyses that show newer agents may offer comparable outcomes with fewer toxicities. A more rigorous appraisal would reference head‑to‑head trials and discuss the trade‑offs inherent in regimen selection.
Sunil Yathakula
10 December 2025Hey guys, great info! Just wanted to add that community support groups can make a huge difference in staying on track with those early appointments. When people share their stories about starting ART quickly, it demystifies the process and encourages others to get tested without fear. Keep spreading the word!
Christopher Burczyk
17 December 2025The clinical evidence supporting same‑day ART initiation is robust; randomized controlled trials have demonstrated increased rates of viral suppression and reduced mortality. It is imperative that healthcare systems streamline confirmatory testing and baseline investigations to avoid unnecessary delays. Additionally, clinicians should be vigilant about potential drug‑drug interactions when prescribing zidovudine alongside other agents, particularly in patients with comorbid conditions.
dennis turcios
23 December 2025While the enthusiasm for early treatment is warranted, the post neglects to address the real‑world challenges of adherence, especially among marginalized populations. Side‑effects, stigma, and access barriers can erode the theoretical benefits outlined. A critical appraisal must incorporate implementation science data that reveal gaps between guideline recommendations and patient experiences.
Felix Chan
30 December 2025Great point, keep it up!
parth gajjar
6 January 2026It’s infuriating how the narrative keeps painting zidovudine as a heroic savior while glossing over the emotional toll of lifelong medication. The drama of “early diagnosis saves lives” feels cheap when patients are left to grapple with side‑effects and the stigma of being labeled “HIV‑positive.” We need more honest discourse that validates the lived experience, not just the virologic numbers.
Maridel Frey
12 January 2026Thank you for highlighting the importance of early testing and prompt treatment initiation. Your insights reinforce the value of integrating comprehensive counseling with clinical care to support patients throughout their journey.