Surgery Risks: What to Know Before Going Under
Facing surgery can feel scary. You want the best outcome with the least trouble. Knowing common risks and how to reduce them gives you control. This page explains the main dangers, practical steps before and after surgery, and what warning signs require quick action.
Common surgical risks and why they happen
Infections at the incision site are one of the most frequent problems. Bacteria can enter during or after the procedure, especially if blood sugar is high or wound care is poor. Bleeding and hematoma (blood pooling) can happen during surgery or in the days after, sometimes needing another procedure.
Anesthesia has its own risks: nausea, sore throat, confusion, and rarely breathing problems or allergic reactions. Blood clots, especially in the legs (DVT), can form when you stay still after an operation. If a clot moves to the lungs, it becomes a pulmonary embolism, which is dangerous and needs immediate care.
Other possible issues include organ or nerve damage depending on the surgery area, delayed healing in smokers or people with diabetes, and unexpected reactions to medications. Risk level depends on the type of surgery, your age, medical history, and how prepared you are.
How to lower your risk before and after surgery
Talk openly with your surgeon. Ask about the specific risks for your procedure and how often they occur in similar patients. Tell your team about all medicines, supplements, allergies, and chronic conditions. Don’t hide tobacco, alcohol, or recreational drug use — those change your risk and the care plan.
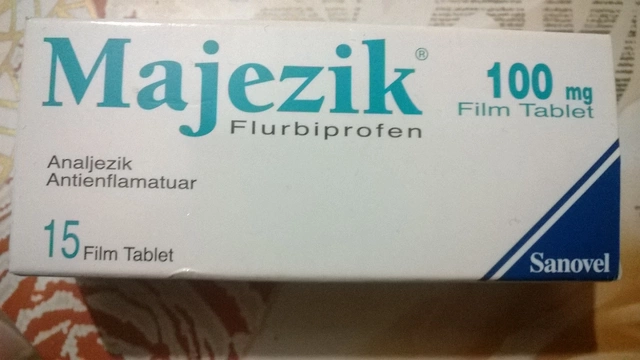
Follow pre-op instructions exactly. You may be told to stop certain blood thinners, adjust diabetes medicine, or fast. Stopping smoking at least a few weeks before surgery cuts the chance of lung and wound problems. Good blood sugar control lowers infection and healing issues for people with diabetes.
After surgery, move as your team allows. Early walking helps prevent clots. Keep the wound clean and dry, and follow dressing change advice. Take prescribed antibiotics or blood thinners when ordered. Watch for fever, increasing pain, redness, pus, sudden shortness of breath, chest pain, or swelling in a leg — these need fast medical attention.
Plan your recovery: arrange help at home, manage pain with the lowest effective dose, and keep follow-up visits. Ask about signs that mean return to the hospital and when to call your surgeon. If you’re unsure, call — it’s better to check early than wait until a small issue grows.
Knowing the risks doesn't mean you should avoid needed surgery. It means you can reduce chances of complications and act fast if something goes wrong. Ask direct questions, prepare well, and follow post-op steps — that’s how you improve outcomes and speed up healing.

Does Anesthesia Cause Blood Clots? Facts About Surgery, Immobility, and Clotting Risk
Wondering if anesthesia causes blood clots? This article uncovers the real connection between anesthesia, surgery, and your risk of developing clots. Get straightforward answers, learn tips to lower clot risks, and see what really triggers clots after an operation. Using real-world examples and facts, we clarify what's myth and what's medical reality—no scare tactics, just useful knowledge.
Health and MedicineLatest Posts
Tags
- online pharmacy
- medication safety
- generic drugs
- medication
- dietary supplement
- side effects
- online pharmacy UK
- drug interactions
- mental health
- impact
- online pharmacies
- statin side effects
- dosage
- generic vs brand
- pediatric antibiotics
- antibiotic side effects
- skin health
- health
- pain relief
- dietary supplements