Potassium spike risks
High potassium, also called hyperkalemia, can climb quickly and cause real danger to your heartbeat and muscles. A sudden potassium spike often feels surprising because early signs are vague: muscle weakness, mild numbness, or feeling unusually tired. Those symptoms can escalate to palpitations, chest tightness, fainting, and even cardiac arrest if not treated. That’s why knowing common triggers, testing steps, and simple prevention tricks matters.
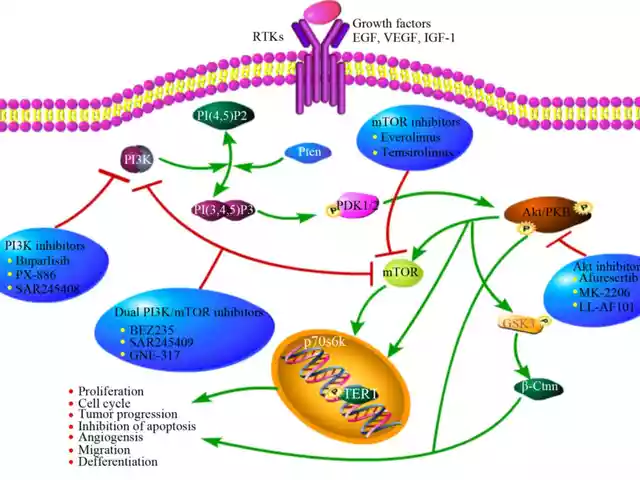
Main causes include poor kidney function, certain prescription drugs, heavy supplementation, and acute tissue breakdown. Kidneys filter potassium; when they fail, potassium stays in the blood. Many medications interfere with potassium balance: ACE inhibitors, angiotensin receptor blockers (ARBs), potassium-sparing diuretics like spironolactone, some beta blockers, and high doses of NSAIDs. Using salt substitutes or over-the-counter potassium supplements adds risk. Severe injuries, burns, or muscle breakdown release potassium from cells and can cause a rapid spike.
Symptoms to watch for
Early signs may be mild, but don’t ignore them. Pay attention to muscle weakness, tingling, or a heavy feeling in your limbs. Heart signs can be subtle: skipped beats, racing heart, or an odd flutter. When chest pain, fainting, or severe shortness of breath occur, head to emergency care. An ECG can show dangerous changes even before you feel severe symptoms.
Testing is simple: a blood potassium level and an ECG. If you’re on drugs that affect potassium, or have kidney disease or uncontrolled diabetes, ask for regular checks. False highs can happen if the blood sample was drawn incorrectly, so labs may repeat a test if the result doesn’t match how you feel. Don’t rely on home scales or symptoms alone — blood tests are the only accurate way to know.
Simple steps to lower risk
Start by reviewing your medication list with a prescriber or pharmacist. Do not stop prescription drugs on your own, but ask whether dose changes or alternative medicines are possible. Avoid taking potassium supplements or using salt substitutes without medical advice. If you eat lots of high-potassium foods, a short diet plan can help until your levels are stable — think smaller portions of bananas, potatoes, avocados, tomatoes, and some beans. Staying hydrated helps kidneys flush potassium when kidney function allows it.
If a spike is confirmed, hospitals can use several tools: calcium to protect the heart, insulin with glucose to shift potassium into cells, diuretics or binding agents to remove potassium, and dialysis for severe cases. Those are medical steps done in a clinic or ER — not at home. If you get sudden weakness, chest discomfort, or fainting, call emergency services. Quick treatment reduces the chance of lasting harm.
People with chronic kidney disease, heart failure, or diabetes should have a clear plan for testing and follow up. Keep a list of prescriptions, over-the-counter drugs, and supplements and bring it to every appointment. Small, practical changes usually prevent dangerous spikes: adjust meds when needed, avoid unnecessary supplements, and get blood tests on schedule. If you worry about your potassium, ask your clinician for a plan you understand and can follow. Early action protects your heart and health.

Alcohol and Spironolactone: Health Risks, Potassium Spikes & Dehydration You Can't Ignore
Mixing alcohol with spironolactone can hit harder than you think, causing potassium spikes, sudden dizziness, and risky dehydration. This article digs into the biology behind these side effects, unpacks warning signs, and delivers practical tips for avoiding complications. You'll find real-life advice, a must-see list of dehydration signals, and facts you won’t stumble upon on a medicine bottle. Stay informed—your kidneys and heart will thank you.
Health and MedicineLatest Posts
Tags
- online pharmacy
- medication safety
- generic drugs
- medication
- dietary supplement
- side effects
- online pharmacy UK
- drug interactions
- mental health
- impact
- online pharmacies
- statin side effects
- dosage
- generic vs brand
- pediatric antibiotics
- antibiotic side effects
- skin health
- health
- pain relief
- dietary supplements