Hypoxia Studies
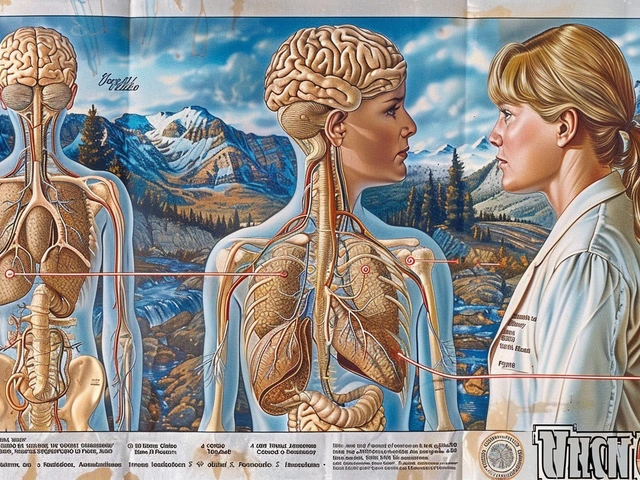
Hypoxia happens when body tissues don't get enough oxygen. It can show up as shortness of breath, confusion, rapid heartbeat, or low energy, but signs vary with cause and severity. People at high altitude, with lung disease, or after a major heart event face higher risk. Knowing common causes helps you act fast and avoid preventable harm.
How hypoxia is studied
Researchers use clear tools: pulse oximeters for quick screening, arterial blood gas tests for exact numbers, and imaging like CT or MRI to check affected organs. Lab studies often use controlled low-oxygen environments to see how cells react, while clinical trials test treatments such as oxygen therapy or drugs that help cells survive low oxygen. Animal models and cell cultures give a controlled view of mechanisms, and human studies show which approaches work in real patients.
Study results usually report oxygen saturation percentages, blood gas levels, and clinical outcomes like recovery time or organ function. When you read research, look for sample size, whether the study was randomized, and how outcomes were measured. Those details tell you how reliable the findings are.
Everyday relevance and treatments
Most cases can be managed with targeted care. Simple steps at home include using a pulse oximeter to monitor oxygen levels and calling your doctor if readings stay below recommended values. Medical treatments range from supplemental oxygen delivered by mask or nasal cannula to more advanced support like noninvasive ventilation or ICU-level care. In some settings, hyperbaric oxygen is used for specific conditions under specialist guidance.
Medications that address underlying causes matter too: bronchodilators and inhaled steroids for COPD, antibiotics for infections that impair breathing, and anticoagulants when blood flow problems cause local hypoxia. Always follow professional advice. Oxygen and some drugs can be harmful if used wrong.
Practical tips that help: keep a record of symptoms and oxygen readings, avoid tobacco and smoke exposure, stay up to date on vaccines that protect the lungs, and talk with your doctor before traveling to high altitude. If you use home oxygen, arrange equipment checks and learn safety rules like avoiding open flames.
When to seek urgent care: severe breathlessness, blue lips or face, fainting, sudden confusion, or sustained low oximeter readings. These are signs that tissues may be starving for oxygen and need immediate evaluation.
Want to learn more about related topics? We cover infection mechanisms, anesthesia risks, and medicines that affect circulation and breathing. Browse our linked articles for practical buying guides, drug safety tips, and clear explainers that make medical choices less confusing.
Typical home oxygen saturation readings are usually 95 to 100 percent in healthy adults. Readings under 90 percent often need medical attention, while some chronic lung patients have lower target ranges set by their doctor. If your oximeter gives odd spikes or falls, check the device fit, warm your hands, and repeat the reading. When research reports improvements, they often quote how many points of saturation rose or how many patients avoided hospital admission.
Learn, ask, act.

The Future of Mountain Sickness Research and Treatment
Hey there, fellow mountain enthusiasts! Soaring to new heights isn't without its challenges, and altitude sickness is a hurdle we all might encounter. I've been delving into the future, uncovering the latest breakthroughs and potential cures that can make our ascents safer. We're talking cutting-edge research and next-gen treatments that promise to keep those dreaded symptoms at bay. Join me as we explore the advancements that could revolutionize our high-altitude adventures and ensure that our mountain experiences remain exhilarating, not nauseating.
Health and WellnessLatest Posts
Tags
- online pharmacy
- medication safety
- generic drugs
- medication
- dietary supplement
- side effects
- online pharmacy UK
- drug interactions
- mental health
- impact
- online pharmacies
- statin side effects
- dosage
- generic vs brand
- pediatric antibiotics
- antibiotic side effects
- skin health
- health
- pain relief
- dietary supplements