Choosing Amount: How to Pick the Right Medication Dose
Giving the wrong dose is a top reason medicines fail or cause harm. Choosing the right amount matters whether it's a daily pill, a liquid for a child, or a short antibiotic course. This page helps you think clearly about dose decisions so you ask better questions and avoid common mistakes.
Key factors to consider
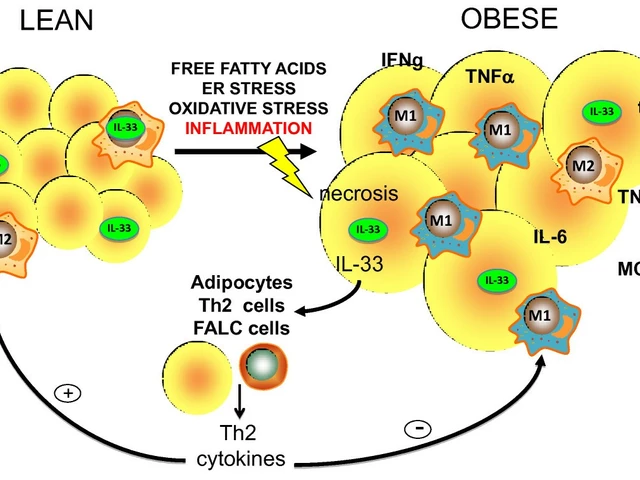
Start with who is taking the drug. Age, weight, pregnancy status, and kidney or liver health change how much medicine your body needs. Some drugs are dosed by weight (especially in children), others use fixed doses for adults. Also check other drugs you take — interactions can raise or lower drug levels, so the right dose for one person might be wrong for another.
Think about the goal of treatment. Are you treating a short infection, managing a long-term condition, or controlling symptoms like pain or anxiety? Acute problems often use higher short-term doses; chronic conditions usually aim for the lowest effective dose to reduce side effects. Ask your prescriber what the treatment target is and how they measure success.
Consider how the medicine is formulated. Liquids, tablets, patches, and injections deliver drugs differently. A crushed pill or cut tablet may change absorption. Extended-release forms are designed to release slowly — splitting them can cause a harmful spike. Always use the form your clinician prescribes.
Practical tips for getting the dose right
Read labels and follow directions exactly. If a label says "take once daily," don’t guess twice daily. Use the right tools: milliliter syringes for liquid medicines and a pill cutter for scored tablets. For children, weigh them and confirm the mg/kg dosing with your pharmacist if you’re unsure.
If your symptoms don’t improve or you get side effects, contact your prescriber before changing the dose. Never double a missed dose unless the instructions tell you to. For short courses like antibiotics, finishing the prescribed amount matters to prevent resistance.
When switching pharmacies or brands, check the strength per unit. Generic names match, but pill sizes and concentrations can differ. Keep a current medication list and share it at every visit. That prevents accidental overdoses and dangerous interactions.
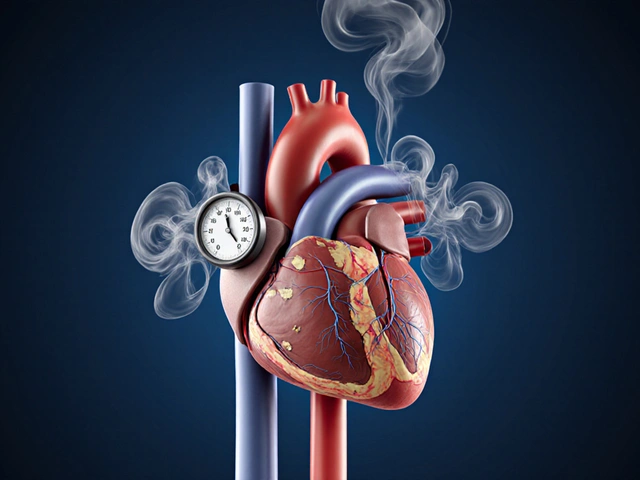
Watch for warning signs. Dizziness, extreme drowsiness, sudden breathing changes, swelling, or rash after a dose are reasons to stop and seek care quickly. For drugs that affect potassium, blood pressure, or blood sugar, regular lab checks are often part of safe dosing.
Final practical step: keep medications stored as directed, and dispose of expired drugs. If cost or access is an issue, ask your provider about lower-dose options or split prescriptions under guidance. Choosing the right amount is a team effort — you, your pharmacist, and your prescriber working together make dosing safer and more effective.
Quick checklist: write down current meds, confirm doses, keep measuring tools, ask about lab tests, and schedule a follow-up if doses change. If you travel or see a new doctor, bring your list and the medication labels. Small steps prevent big mistakes today.
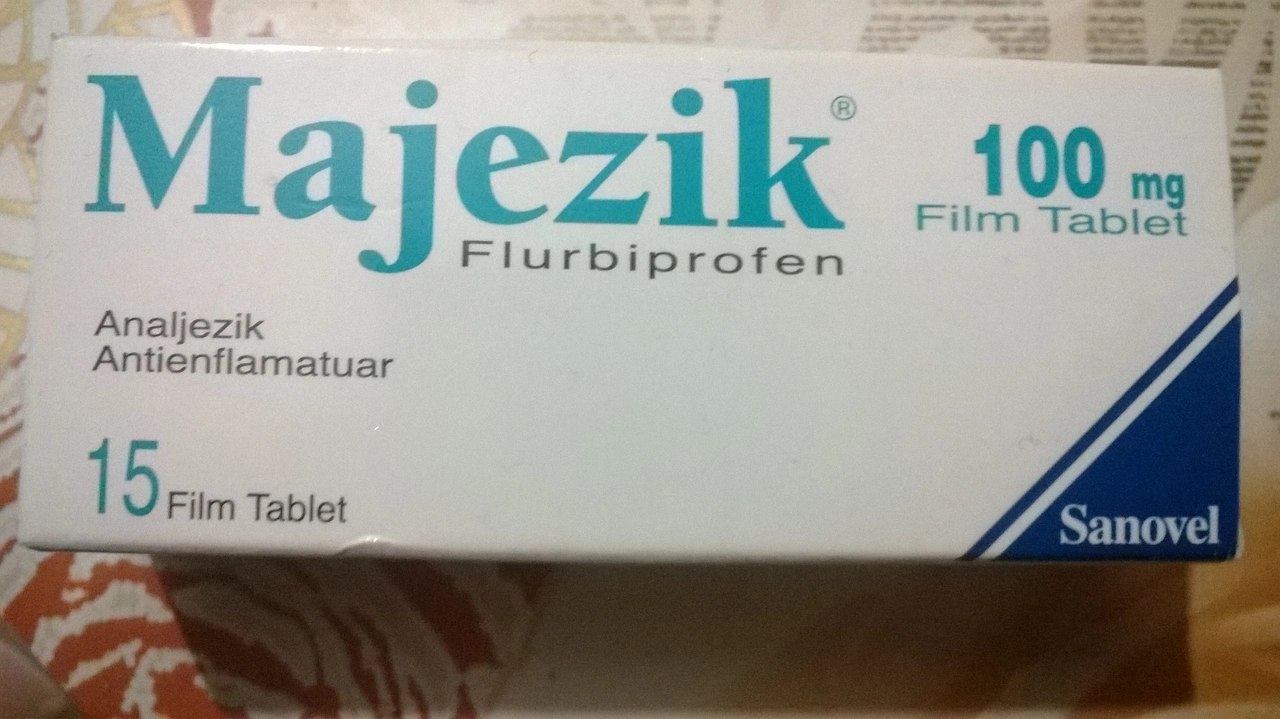
Flurbiprofen Dosage: How to Choose the Right Amount for Your Pain
In today's blog post, we'll be discussing Flurbiprofen dosage and how to choose the right amount for your pain relief. Flurbiprofen is a nonsteroidal anti-inflammatory drug (NSAID) that helps reduce inflammation and alleviate pain. It's crucial to follow your doctor's recommendations for the correct dosage, as it may vary based on factors such as age, weight, and the severity of pain. Remember, taking more than the recommended dose can lead to potential side effects and complications. Stay tuned for a more in-depth look at Flurbiprofen and tips on managing your pain effectively.
Health and WellnessLatest Posts
Tags
- online pharmacy
- medication safety
- generic drugs
- medication
- dietary supplement
- side effects
- online pharmacy UK
- drug interactions
- mental health
- impact
- online pharmacies
- statin side effects
- dosage
- generic vs brand
- pediatric antibiotics
- antibiotic side effects
- skin health
- health
- pain relief
- dietary supplements