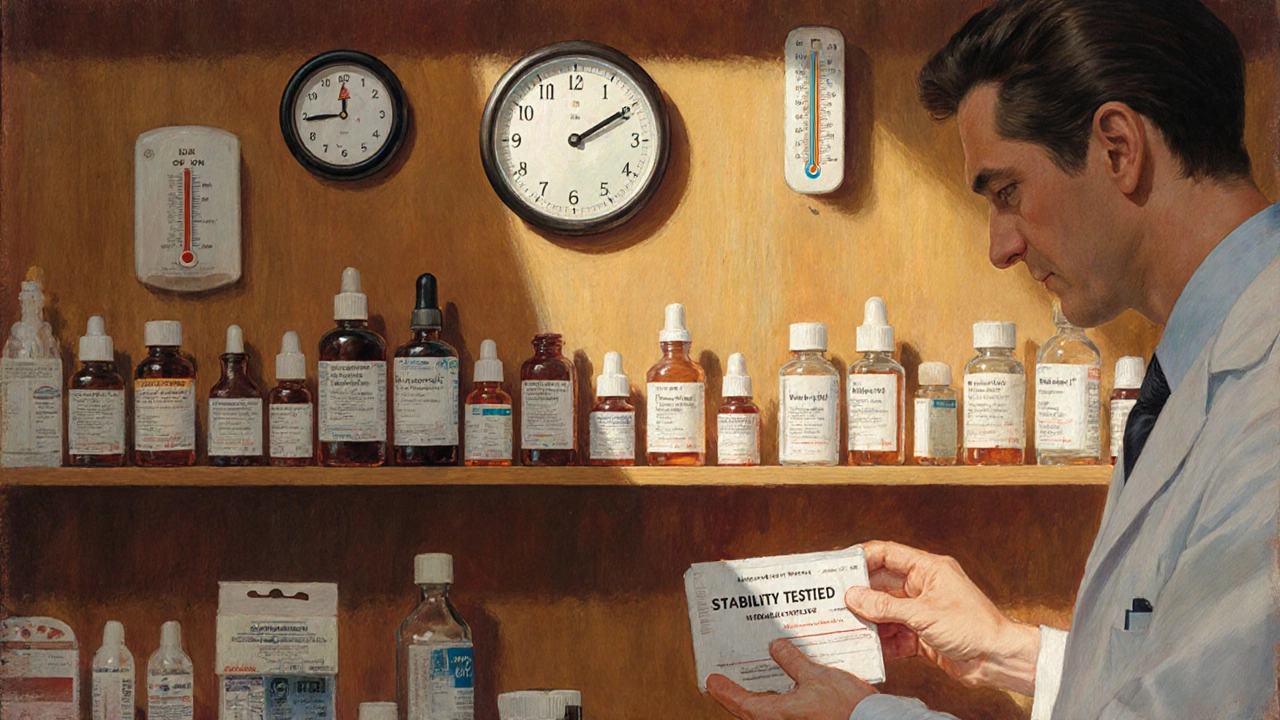
When you take a pill, injection, or nasal spray, you expect it to work the same way on the last day of its shelf life as it did on the first. That’s not luck-it’s the result of strict stability testing under controlled temperature and time conditions. Without these tests, drugs could lose potency, break down into harmful substances, or fail to dissolve properly in your body. This isn’t optional. It’s a legal requirement enforced by global regulators like the FDA and EMA. And at the heart of it all are precise numbers: 25°C, 40°C, 6 months, 12 months. Get those wrong, and a whole product line can be pulled from shelves.
Why Temperature and Time Matter in Stability Testing
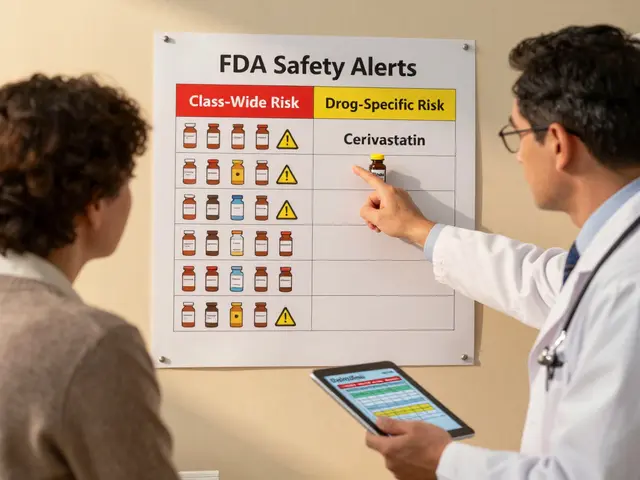
Drugs don’t sit still on a shelf. Heat, moisture, and time slowly change their chemistry. A tablet might absorb water and crumble. A liquid might separate. A biologic might clump together and become unsafe. Stability testing simulates how a drug behaves over its entire lifespan under real-world conditions. It answers two critical questions: How long can you store it? And under what conditions? The International Council for Harmonisation (ICH) set the global standard with ICH Q1A(R2), published in 2003. It’s still the rule today. The FDA, EMA, Health Canada, and Japan’s PMDA all follow it. That means if you’re making a drug for global markets, you don’t design separate tests for each country-you follow one set of rules. But that doesn’t make it simple. The conditions are exact, the timelines are long, and the consequences of failure are severe. In 2022 alone, the FDA issued 27 warning letters over stability testing failures.Long-Term Testing: The Real-Time Clock
Long-term testing is the backbone of stability. It’s where you track how a drug actually degrades over time under normal storage conditions. There are two main options, both defined by ICH Q1A(R2):- 25°C ± 2°C with 60% RH ± 5% RH
- 30°C ± 2°C with 65% RH ± 5% RH
Accelerated Testing: The Speed Run
You can’t wait three years to launch a drug. That’s where accelerated testing comes in. It’s a high-stress test designed to predict long-term behavior in a fraction of the time. The global standard is simple: 40°C ± 2°C with 75% RH ± 5% RH for 6 months. This isn’t meant to be realistic-it’s meant to be extreme. It simulates what might happen if a shipment got stuck in a hot warehouse or a warehouse’s AC failed. If the drug passes this test without major changes, it’s a strong indicator it’ll last under normal conditions. Here’s the catch: the 6-month accelerated test is only valid if you also have long-term data. If your long-term study is at 25°C, you must run an intermediate test at 30°C/65% RH for 6 months to confirm the results aren’t misleading. If your long-term study is already at 30°C, the intermediate test isn’t needed.Refrigerated and Frozen Products: Different Rules
Not all drugs are stored at room temperature. Insulin, vaccines, and many biologics need refrigeration-or even freezing. Their stability rules are different. For refrigerated products (2-8°C), the long-term condition is 5°C ± 3°C for 12 months. The accelerated condition? Not 40°C. That would destroy them. Instead, it’s 25°C ± 2°C with 60% RH ± 5% RH for 6 months. This mimics what happens if a fridge breaks and the product warms up. For frozen products, the long-term condition is typically -20°C or colder. Accelerated testing here is trickier. It often involves repeated freeze-thaw cycles to simulate handling during shipping. There’s no single ICH rule yet-this is still evolving, especially for mRNA vaccines and cell therapies.
Climatic Zones: One Size Doesn’t Fit All
The world isn’t one climate. ICH recognizes five zones, each with different temperature and humidity profiles:- Zone I (Temperate): 21°C / 45% RH
- Zone II (Mediterranean/Subtropical): 25°C / 60% RH
- Zone III (Hot-Dry): 30°C / 35% RH
- Zone IVa (Hot-Humid/Tropical): 30°C / 65% RH
- Zone IVb (Hot/Higher Humidity): 30°C / 75% RH
What Counts as a “Significant Change”?
The biggest gray area in stability testing isn’t the temperature-it’s the judgment call. ICH Q1A(R2) says a product has failed if there’s a “significant change” in any critical quality attribute. But it doesn’t define what “significant” means. Typically, it’s:- A 5% change in assay (potency)
- A 10% increase in impurities
- Failure to meet dissolution specs
- Physical changes like discoloration, clumping, or leakage
Real-World Challenges: Chamber Failures and Delays
It sounds simple: put the drug in a box, wait, test. But in practice, it’s messy. A 2023 survey of 142 stability professionals found that 78% had experienced at least one temperature excursion-meaning the chamber went outside the ±2°C range. One 3-hour spike at 42°C can ruin a 12-month study. That means restarting the clock, delaying a product launch, and losing millions. Humidity control is another headache. In dry climates, maintaining 60% RH requires adding water vapor. In humid ones, you need to remove it. Many labs use dual-loop systems to keep RH stable within ±3%, down from ±8% in older setups. And then there’s the wait. A typical long-term study takes 12-24 months to complete. For many small biotechs, this delay is the biggest bottleneck to getting a drug to market. One CPT Labs survey showed 67% of companies had at least one project delayed because of stability testing.
What’s Changing? The Future of Stability Testing
The ICH Q1A(R2) guidelines are 20 years old. The world has changed. We now have mRNA vaccines, antibody-drug conjugates, and continuous manufacturing. These products don’t degrade the way old tablets do. The FDA is running a pilot program using real-time monitoring (PAT) to predict stability without waiting months. Some companies are using predictive models-running tests at 50°C, 60°C, even 80°C-to forecast shelf life in weeks instead of years. In 2022, 74% of top pharma companies used these accelerated predictive studies. But regulators are cautious. The EMA rejected eight model-based submissions in 2022-2023 because they didn’t trust the math. The industry is pushing for change. The ICH Q1F update, expected in late 2024, will address complex products like ADCs and cell therapies. For now, the rules are clear: 25°C or 30°C, 60% or 65% RH, 12 months minimum, 40°C for acceleration. But the future? It’s moving toward smarter, faster, risk-based testing. The goal isn’t just compliance-it’s predicting failure before it happens.How to Get Started
If you’re new to stability testing:- Define your product’s intended storage conditions based on target markets.
- Choose your long-term and accelerated conditions from ICH Q1A(R2).
- Qualify your environmental chambers-follow ASTM E1993-19 for IQ/OQ/PQ.
- Design a testing schedule: 0, 3, 6, 9, 12, 18, 24, 36 months.
- Run a pilot study to catch early degradation.
- Document everything: protocols, raw data, annual reports.
- Work with a regulatory consultant if you’re unsure about “significant change” thresholds.





Lisa Lee
23 November 2025This whole system is a joke. We’re spending millions to test pills at 25°C when half the world lives in 40°C heat and 80% humidity. Why does Canada get to dictate how India stores medicine? The FDA and EMA are just protecting their own pharma empires while people in the Global South get degraded, ineffective drugs. It’s colonialism with a lab coat.
Kezia Katherine Lewis
23 November 2025While I appreciate the thorough overview of ICH Q1A(R2), I’d like to emphasize the critical distinction between Zone II and Zone IVa conditions-particularly regarding the hygroscopic behavior of amorphous APIs. The 60% RH threshold is not arbitrary; it’s empirically derived from water activity thresholds that trigger phase transitions in crystalline lattices. Failure to account for this in accelerated studies can lead to non-linear degradation kinetics, invalidating predictive models. Regulatory submissions must include RH-controlled DSC and XRPD data to substantiate stability claims.
Dalton Adams
24 November 2025Ugh, another post pretending this is ‘science.’ Let’s be real-this whole process is bureaucratic theater. 40°C for 6 months? That’s not ‘accelerated,’ that’s just arson with a thermometer. And don’t get me started on the 5% potency drop rule-some drugs are still effective at 30% loss! I’ve seen data where a 4.9% drop got a product shelved while a 12% drop in a competitor’s product got approved because ‘the clinical impact was negligible.’ HA. Regulators don’t care about science-they care about paperwork. Also, who writes ‘±2°C’ like it’s a math equation? 😒
Matthew Mahar
25 November 2025Okay I know this sounds wild but what if we just… stopped testing for 12 months? Like… what if we used AI to predict degradation based on molecular structure and real-time sensor data from shipping containers? I read this paper where they trained a model on 2000+ stability datasets and it predicted shelf life within 2 weeks of actual results. Maybe we’re over-engineering this? I’m not saying ditch the rules… but maybe… we could… kinda… evolve? 🤔
Ragini Sharma
26 November 2025bro i just work in a lab in delhi and we use 30c/65%rh for everything… but the corporate HQ in nyc keeps sending us their 25c protocols… so we just… fake the data? lol. also why do we test at 9 months? no one checks at 9 months. only 0, 6, 12. who even cares about 9? 😅
Linda Rosie
28 November 2025Stability testing is not optional. It is a foundational pillar of patient safety.
Vivian C Martinez
28 November 2025Great breakdown! I especially appreciate the note about real-time monitoring pilots-this is where the field is heading. If you're just starting out, don’t get overwhelmed by the 36-month timelines. Focus on nailing your chamber qualification and sampling schedule first. You’ve got this. 💪
Ross Ruprecht
29 November 2025So basically we’re all just waiting around for 3 years so some guy in a lab coat can check if a pill still looks like a pill? Cool. I’ll just go back to my nap.