Imagine taking a natural supplement to feel better-only to find out it’s quietly making your blood pressure medicine, birth control, or transplant drug useless. That’s not a hypothetical. It’s happening to people right now, and St. John’s Wort is one of the most dangerous offenders.
What Is St. John’s Wort, Really?
St. John’s Wort (Hypericum perforatum) is a yellow-flowered plant that’s been used for centuries to lift mood. Today, it’s sold as capsules, tablets, or liquid drops in pharmacies and health stores. In Germany, it’s so common that one in five people with mild depression take it instead of prescription antidepressants. In the U.S., about 4.7% of adults use it-mostly women between 35 and 54.
But here’s the catch: it’s not harmless. Unlike real drugs, herbal supplements like St. John’s Wort don’t go through strict testing before hitting shelves. The FDA doesn’t approve them. No one checks if the bottle actually contains what it claims. And no one tells you-until it’s too late-that this plant can wreck your medication.
How It Breaks Your Prescription Drugs
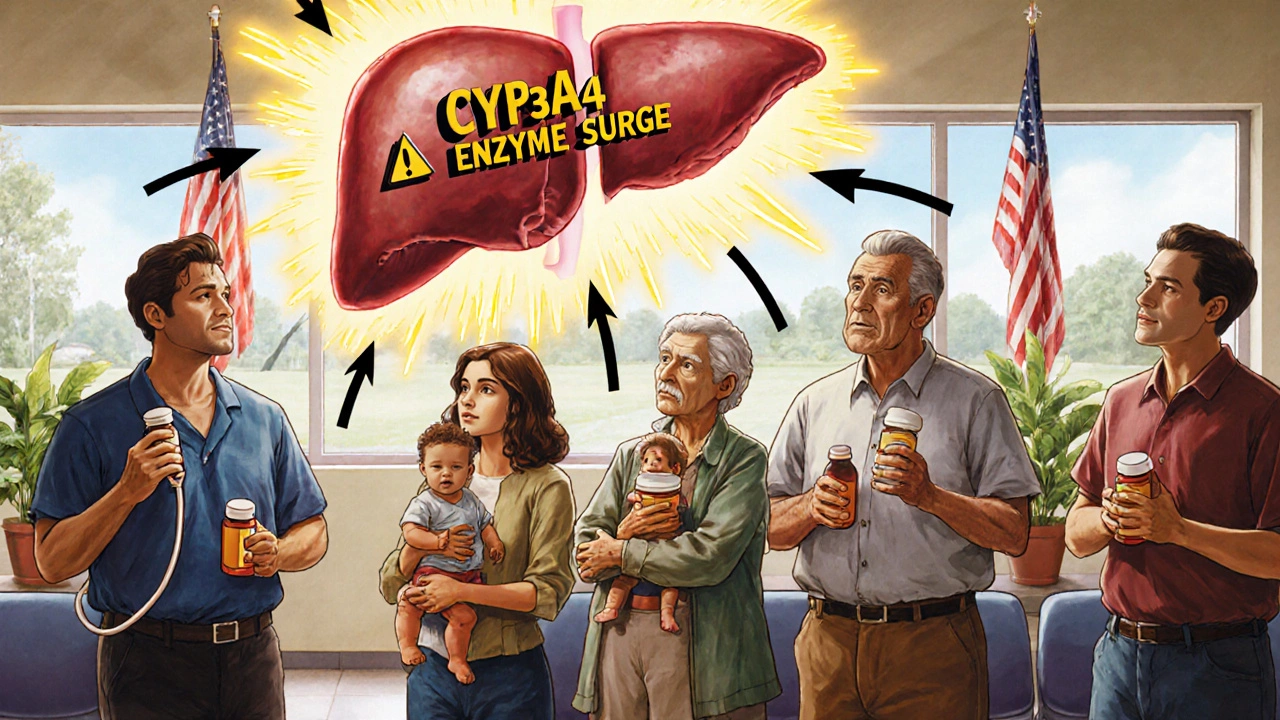
St. John’s Wort doesn’t just interact with drugs. It actively dismantles them. The main culprit is a compound called hyperforin. This chemical turns on a switch in your liver called the pregnane-X-receptor (PXR). When activated, it tells your body to produce more enzymes-specifically CYP3A4, CYP2C9, and CYP1A2-that break down medications faster than normal.
Think of it like this: your body is a factory. Your prescription drug is a delivery truck. St. John’s Wort is a boss who suddenly hires 10 extra workers to unload trucks faster. The result? The drug never reaches its target. It’s gone before it can do its job.
This isn’t theoretical. In 2019, a 34-year-old woman had a kidney transplant and was on tacrolimus-a drug that keeps her body from rejecting the new organ. Her levels were stable. Then she started taking St. John’s Wort. Eight weeks later, her tacrolimus levels crashed. Her body rejected the kidney. She ended up back in the hospital. This exact scenario has happened dozens of times.
Medications That Can Fail Because of St. John’s Wort
Over 50 prescription drugs are known to interact with St. John’s Wort. Some of the most dangerous include:
- Immunosuppressants like cyclosporine and tacrolimus-used after organ transplants. If these drop, your body attacks the new organ.
- Anticoagulants like warfarin. A 2000 case report showed a patient’s INR (a measure of blood clotting) dropped from 2.5 to 1.4 in just 10 days after starting St. John’s Wort. That’s the difference between being protected from clots and risking a stroke.
- Oral contraceptives. At least 17 women reported unintended pregnancies after combining St. John’s Wort with birth control pills. The herb speeds up estrogen breakdown. Your pill stops working.
- Antidepressants like SSRIs (Prozac, Zoloft). Mixing them with St. John’s Wort can trigger serotonin syndrome-a rare but deadly condition where your brain gets flooded with serotonin. Symptoms: high fever, seizures, irregular heartbeat. It kills.
- HIV medications like protease inhibitors. If these levels drop, the virus rebounds. Drug resistance follows. Treatment fails.
- Painkillers like oxycodone, methadone, and tramadol. St. John’s Wort reduces their pain-relieving effect. People end up in agony because their meds aren’t working.
The European Medicines Agency says St. John’s Wort should never be taken with any drug that has a narrow therapeutic index-meaning the difference between a safe dose and a toxic one is tiny. That’s most of the drugs listed above.

Why People Think It’s Safe
“It’s natural,” people say. “It’s been used for centuries.” But so was arsenic. And lead. And tobacco.
St. John’s Wort feels safe because it doesn’t cause drowsiness like some antidepressants. It doesn’t cause weight gain. It’s marketed as “gentle.” But that’s the trap. The danger isn’t obvious. You don’t feel sick right away. You just notice your birth control isn’t working. Or your blood pressure is climbing. Or your pain is back.
Studies show it takes 3 to 6 weeks for people to realize something’s wrong. By then, the damage is done. The enzyme induction peaks around day 10-and lasts for two weeks after you stop taking it. So even if you quit the herb before surgery or starting a new drug, you’re still at risk.
What You Should Do Instead
If you’re considering St. John’s Wort for depression or anxiety, pause. Ask yourself: are you on any prescription meds? Even one? If yes, don’t take it.
There are safer alternatives. SAM-e has almost no known interactions. 5-HTP is another option, though less studied. Neither triggers the liver enzymes like St. John’s Wort does.
If you’re already taking it, talk to your pharmacist. Bring your bottle. Ask: “Which of my meds could this be affecting?” Pharmacists are trained to spot these interactions. They see them every day.
If you’re on a transplant drug, anticoagulant, or HIV treatment-stop St. John’s Wort immediately. Don’t wait. Don’t taper. Just quit. Then get your drug levels checked within 72 hours.
The Bigger Problem: Lack of Warning Labels
In the U.S., St. John’s Wort labels often say “may interact with medications.” That’s it. No list. No urgency. No clarity.
In Europe, labels must warn about 12 specific drug classes. In the U.S., you’re on your own.
And here’s the worst part: many people don’t even tell their doctors they’re taking it. A 2017 study found that 60% of patients using herbal supplements didn’t mention them during appointments. Doctors assume you’re only on prescription meds. They don’t think to ask.
If you’re taking St. John’s Wort, tell your doctor. Write it down. Bring the bottle. Don’t assume they’ll know.
What’s Changing Now?
Researchers are working on a solution: hyperforin-free extracts. Early studies show these versions don’t trigger the same enzyme response. One 2022 study found a 90% drop in CYP3A4 induction. That’s promising.
But they’re not on the market yet. And even if they were, you’d still need to know what’s in your bottle. Most products don’t list hyperforin content. You can’t tell if you’re getting the dangerous kind.
The FDA issued updated guidance in March 2023 calling St. John’s Wort a “high-risk supplement.” That’s the first time they’ve singled out a single herb like this. It’s a warning. But it’s not stopping sales.
Global sales have dropped 37% since 2000, mostly because people are learning the truth. In the U.S., usage is falling. In Europe, it’s still popular-but only where warnings are clear and doctors are vigilant.
Final Reality Check
St. John’s Wort isn’t evil. It can help mild depression. Some people swear by it. But it’s not a gentle herb. It’s a biochemical disruptor. And if you’re on any prescription medication, it’s not worth the risk.
You don’t need to be a scientist to understand this: if your drug has a narrow therapeutic window-if it’s life-saving-don’t mix it with anything unless your doctor says it’s safe. And even then, get blood tests.
There’s no shortcut to safety. No natural loophole. No “it’s just a herb” excuse. Your body doesn’t care if something is labeled “natural.” It only cares about chemistry.
Ask yourself: is feeling a little better worth risking your transplant, your birth control, your pain control, or your life?
If the answer isn’t a clear yes, then don’t take it.
Can St. John’s Wort make birth control fail?
Yes. St. John’s Wort speeds up how fast your body breaks down estrogen and progestin-the active ingredients in most birth control pills, patches, and rings. This can drop hormone levels below the threshold needed to prevent pregnancy. At least 17 women have reported unplanned pregnancies after using it. If you’re on hormonal birth control, avoid St. John’s Wort completely.
How long does it take for St. John’s Wort to affect my medications?
The enzyme-inducing effects start within 5-7 days, peak around day 10, and can last up to two weeks after you stop taking it. That means even if you quit the herb before surgery or starting a new drug, you’re still at risk for at least two weeks. Don’t assume stopping it quickly fixes the problem.
Is St. John’s Wort safe if I’m not on any medications?
If you’re not taking any prescription drugs, over-the-counter meds, or supplements, it’s generally safe for short-term use in mild depression. But even then, side effects like dry mouth, dizziness, or increased sun sensitivity can occur. And if you start any new medication later-even an antibiotic or painkiller-you’ll need to stop St. John’s Wort immediately.
Can I take St. John’s Wort with antidepressants?
No. Combining St. John’s Wort with SSRIs, SNRIs, or MAO inhibitors can cause serotonin syndrome-a potentially fatal condition. Symptoms include confusion, rapid heart rate, high fever, muscle rigidity, and seizures. The Mayo Clinic and FDA both warn against this combination. There is no safe way to mix them.
What should I do if I’ve been taking St. John’s Wort with my prescription drugs?
Stop taking St. John’s Wort immediately. Contact your doctor or pharmacist. Ask for blood tests to check levels of your medications-especially if you’re on transplant drugs, blood thinners, or HIV meds. Don’t wait for symptoms. Many interactions show no warning signs until it’s too late. Keep the bottle to show your provider exactly what you took.







Mark Kahn
21 November 2025Just wanted to say thanks for laying this out so clearly. I’ve been taking St. John’s Wort for mild anxiety and had no idea it could mess with my blood pressure med. I’m stopping it today and going to see my pharmacist tomorrow. You just might’ve saved my life.
Stay safe out there, folks.
Daisy L
23 November 2025Oh my GOD. I’ve been taking this stuff for YEARS!! And now I find out it’s basically a silent assassin for my birth control?!? I’m 32, single, and just had my first unplanned pregnancy-AND I THOUGHT IT WAS ‘NATURAL’?!?!?!!?!!? THE FDA IS ASLEEP!! THE PHARMACIES ARE LYING!! THIS IS A COVER-UP!!
WHO’S PROFITING FROM THIS?!?!?!!?!!? I DEMAND ANSWERS!!
Anne Nylander
24 November 2025OMG I JUST READ THIS AND I’M SO GLAD I DID!! I WAS THINKING ABOUT TRYING ST. JOHNS WORT FOR MY DEPRESSION!! THANK YOU FOR THE WARNING!! I’M GOING TO TALK TO MY DOCTOR TOMORROW!! YOU’RE THE BEST!!
STAY STRONG!! YOU GOT THIS!!
Clifford Temple
26 November 2025So let me get this straight-you’re telling me some hippie herbalist from the 1800s knows more about my liver than modern science? That’s why America’s falling apart. We let people self-diagnose with tea leaves and call it ‘wellness.’ This isn’t medicine. It’s a cult. And now you’re telling me we’re letting this poison be sold next to candy bars? What kind of country are we?
I say ban it. Ban all of it. No more ‘natural’ nonsense. If it’s not FDA-approved, it’s not allowed on the shelf. Period.
Corra Hathaway
26 November 2025Okay but can we just take a second to appreciate how wild it is that we trust a pill made in a lab with 17 chemicals more than a plant that’s been around since the Roman Empire? 🤔
Also-serotonin syndrome? That sounds like a Marvel villain’s origin story. 😅
Anyway-thank you for this. I’m deleting my St. John’s Wort order right now. And yes, I’m telling my mom. She’s been taking it since 2012. 😬
Shawn Sakura
27 November 2025Thank you for this post. I am a nurse, and I see this every week. Patients come in with perfectly stable INR levels, then suddenly have a stroke because they started ‘natural mood support.’
It is not a miracle herb. It is a biochemical weapon. And we are not educating people enough. Please, if you’re reading this-ask your doctor. Bring the bottle. Even if you think it’s ‘just a supplement.’
Small steps save lives.
Paula Jane Butterfield
29 November 2025As someone who grew up in a family that used herbal remedies for everything-tea for colds, turmeric for pain, St. John’s Wort for sadness-I didn’t realize how dangerous this could be until my cousin lost her kidney transplant because of it.
It’s not about being ‘anti-natural.’ It’s about being informed. Just because something comes from the earth doesn’t mean it’s gentle. Poison ivy is natural too.
If you’re taking anything prescription-please, please, please check with your pharmacist. They’re the real heroes here.
And if you’re feeling low? There are safer options. You’re worth more than a risky shortcut.
Julia Strothers
29 November 2025This is all a psyop. The pharmaceutical companies own the FDA. They don’t want you to know that a $3 herb can replace their $200/month antidepressants. That’s why they let this warning be buried under 3 paragraphs of ‘may interact.’
They’ve been suppressing hyperforin-free extracts for 15 years because if people knew they could get the benefits without the danger, the whole profit model collapses.
Wake up. This isn’t science. It’s capitalism. And you’re the product.
Erika Sta. Maria
30 November 2025But what if the real danger is not the herb, but our obsession with control? We want to quantify everything-enzyme levels, drug concentrations, therapeutic windows. But nature doesn’t work like that. St. John’s Wort is not a ‘drug.’ It’s a conversation between your body and the earth. You’re reducing a sacred plant to a biochemical grenade.
Perhaps the problem isn’t the herb-it’s that we’ve forgotten how to listen to our bodies without a lab report.
Also, I took it with my antidepressants for 3 years. No serotonin syndrome. Just peace. Coincidence? Or wisdom?
Nikhil Purohit
1 December 2025Hey, I’m from India and we’ve used Hypericum for generations in Ayurveda-mostly for wounds and mood. But we never mixed it with Western meds. Always left a gap. I think the real issue here is cultural ignorance, not the herb itself.
Also, I asked my pharmacist here-she said if you’re on anything important, wait 14 days after stopping St. John’s Wort before starting the new med. That’s the key. Not fear. Just timing.
Thanks for the post. Really helpful.