Antipsychotic Medication Comparison Tool
Select your top priorities to see which antipsychotics may be most effective for your situation.
What are your top treatment priorities?
Clozapine isn’t your typical antipsychotic. While most drugs for schizophrenia try to calm the brain with a broad stroke, clozapine works differently - often when everything else has failed. It’s the last-resort medication, but for some people, it’s the only thing that brings back their sense of self. If you or someone you care about has tried multiple antipsychotics without success, understanding how clozapine compares to others isn’t just helpful - it could be life-changing.
Why Clozapine Is Different
Clozapine was first approved in the 1970s, but its use was nearly halted after a rare but deadly side effect - agranulocytosis - caused blood cell counts to crash. That risk led to strict monitoring rules that still exist today: every patient on clozapine must get weekly blood tests for the first six months, then every two weeks after that. It’s a hassle, but it saves lives.
What makes clozapine stand out isn’t its side effects - though they’re serious - it’s its effectiveness. Studies show that about 30% to 50% of people with treatment-resistant schizophrenia respond to clozapine when other drugs didn’t work. That’s not a small number. That’s the difference between being stuck in a hospital and returning home.
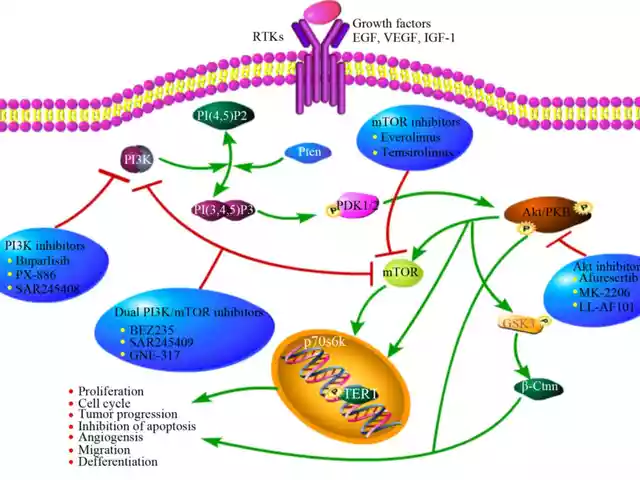
Unlike other antipsychotics that mainly block dopamine, clozapine also affects serotonin, acetylcholine, and norepinephrine. This broader action helps with negative symptoms like emotional flatness, social withdrawal, and lack of motivation - things other drugs often ignore.
Common Alternatives to Clozapine
If clozapine isn’t right for you, there are other options. But not all are equal. Here are the most commonly prescribed alternatives and how they stack up.
- Risperidone: Often used as a first-line treatment. It’s effective for hallucinations and delusions, but less so for negative symptoms. Weight gain and movement problems like tremors are common.
- Olanzapine: Similar in effectiveness to clozapine for positive symptoms, but causes more weight gain and metabolic issues. It’s easier to use because it doesn’t need blood monitoring.
- Quetiapine: Popular for its calming effect, especially at night. It’s less likely to cause movement side effects, but can lead to drowsiness and low blood pressure.
- Aripiprazole: A partial dopamine activator. It’s less likely to cause weight gain or sedation, but can cause restlessness and anxiety in some.
- Paliperidone: The active metabolite of risperidone. Longer-lasting, given as a monthly injection. Good for adherence, but still carries risks of weight gain and high prolactin levels.
None of these match clozapine’s ability to reduce treatment-resistant psychosis. But they’re safer, easier to manage, and often tried first - not because they’re better, but because they’re less risky.
Side Effects: The Trade-Offs
Clozapine’s side effects are why doctors hesitate. But so are the side effects of other drugs. Here’s how they compare:
| Side Effect | Clozapine | Risperidone | Olanzapine | Quetiapine | Aripiprazole |
|---|---|---|---|---|---|
| Agranulocytosis (dangerous low white blood cells) | High risk - requires weekly blood tests | Very low risk | Very low risk | Very low risk | Very low risk |
| Weight gain | High | Moderate | Very high | Moderate to high | Low |
| Sedation | High | Moderate | High | Very high | Low |
| Movement disorders (tremors, stiffness) | Low | High | Moderate | Low | Moderate |
| Metabolic issues (diabetes, high cholesterol) | High | Moderate | Very high | Moderate | Low |
| Effect on negative symptoms | Strong | Weak | Moderate | Moderate | Moderate |
Many people choose clozapine not because they want to deal with blood tests, but because they’ve already tried the others and still hear voices, feel paranoid, or can’t get out of bed. The trade-off isn’t just medical - it’s personal.

Who Benefits Most From Clozapine?
Clozapine isn’t for everyone. But it’s the only drug proven to help people who’ve tried at least two other antipsychotics without relief. That’s called treatment-resistant schizophrenia. If you’ve been on risperidone, olanzapine, or quetiapine for months and still struggle with hallucinations or deep apathy, clozapine should be discussed.
It’s also the only antipsychotic shown to reduce suicide risk in people with schizophrenia. That’s not a minor point. Suicide is the leading cause of early death in this population. For someone who’s felt hopeless for years, clozapine might be the only thing that brings back the will to live.
It’s not a cure. But for many, it’s the difference between surviving and living.
When to Avoid Clozapine
Clozapine isn’t safe for everyone. You should avoid it if:
- You have a history of severe bone marrow problems or previous agranulocytosis
- You’re taking other medications that suppress white blood cells (like some chemotherapy drugs)
- You have untreated seizures or a history of epilepsy
- You have severe heart disease or uncontrolled low blood pressure
- You can’t commit to regular blood testing - missing even one test can be dangerous
Also, clozapine isn’t usually started in older adults or people with dementia-related psychosis. The risks outweigh the benefits in those cases.
What Happens If You Stop Clozapine?
Stopping clozapine suddenly can cause rebound psychosis - meaning symptoms return faster and worse than before. That’s why tapering off takes weeks, sometimes months, under close supervision.
Even after stopping, the risk of agranulocytosis can linger for weeks. That’s why blood tests continue for at least four weeks after the last dose. Many people don’t know this - and that’s dangerous.
If you’re thinking of stopping because of side effects, talk to your doctor first. There are ways to manage weight gain, sedation, or drooling - without giving up the only medication that’s working.

Real Stories, Real Choices
In Bristol, a 34-year-old man named Mark tried five antipsychotics over seven years. He was hospitalized three times. He couldn’t hold a job. His family stopped visiting because he didn’t recognize them.
After starting clozapine, his hallucinations faded. He started cooking again. He went back to college part-time. He still gets blood tests every two weeks. He still feels tired. But he says, “I’m not a ghost anymore.”
That’s the power of clozapine. It doesn’t fix everything. But for people who’ve lost everything, it gives back a piece of themselves.
Next Steps: Talking to Your Doctor
If you’re considering clozapine, here’s what to ask:
- Have I tried at least two other antipsychotics at adequate doses for long enough?
- Do I have any conditions that make clozapine unsafe?
- Can I commit to weekly blood tests for the first six months?
- What support is available to help manage side effects like weight gain or sleepiness?
- What happens if I miss a blood test?
Don’t be afraid to push for a referral to a specialist. Clozapine is often overlooked because of its complexity - not because it’s ineffective. The right person, at the right time, can change everything.
Frequently Asked Questions
Is clozapine better than other antipsychotics?
Clozapine is more effective than other antipsychotics for treatment-resistant schizophrenia - especially for negative symptoms and reducing suicide risk. But it’s not better for everyone. It carries serious risks like agranulocytosis and requires strict monitoring. For people who haven’t responded to other drugs, it’s often the best option. For others, safer alternatives may be more appropriate.
Can clozapine be used as a first-line treatment?
No. Guidelines from NICE and the American Psychiatric Association recommend clozapine only after at least two other antipsychotics have failed. It’s not a first-choice drug because of its risks and monitoring requirements. But that doesn’t mean it’s a last hope - it’s the most effective tool for specific cases.
How long does it take for clozapine to work?
Some people notice improvements in agitation or sleep within a week. But full effects - especially on negative symptoms like lack of motivation - can take 3 to 6 months. Patience is key. Stopping too early means missing out on the full benefit.
Do I have to take clozapine for life?
Not necessarily. Some people stabilize and stay on clozapine long-term. Others reduce their dose or switch to another medication after years of stability. But stopping suddenly can trigger severe relapse. Any change must be done slowly and under medical supervision.
What if I can’t afford regular blood tests?
In the UK, clozapine monitoring is covered by the NHS. If you’re outside the UK, check with your provider or local mental health services. Some clinics offer free or low-cost blood testing for clozapine patients. Never skip tests because of cost - the risk of agranulocytosis is life-threatening.





Donald Sanchez
19 November 2025bro clozapine is basically the dark mode of antipsychotics 😅 i tried risperidone, it made me feel like a zombie with a side of donut belly. clozapine? yeah i get the drool and the blood tests… but at least i can remember my mom’s face again. also, who else has had that moment where you’re just sitting there and you realize… you haven’t heard the voices for 3 days? 🥲
Greg Knight
20 November 2025I just want to say that if you’re on the fence about clozapine because of the blood tests, please don’t let that scare you off. I’ve been on it for 8 years now. Every two weeks, I go to the clinic, they poke my finger, I get a sticker, and I go about my day. The real sacrifice isn’t the blood tests-it’s the years you waste on meds that don’t work while your life slips away. I used to sit in my apartment for months without talking to anyone. Now I tutor kids in math. I’m not ‘cured,’ but I’m here. And that’s everything. Don’t let bureaucracy rob you of your humanity.
rachna jafri
22 November 2025They don’t want you to know this but clozapine was developed by Big Pharma to control the brown people. Why do you think they only push it in poor neighborhoods? The blood tests? A trap. The real agenda is to monitor your DNA through the white blood cells. I read a paper once-well, someone quoted a paper-saying the government uses it to track dissent. My cousin in Delhi got kicked off it because they said his ANC was low… but he never even left India. Coincidence? I think not. 🇮🇳✊
darnell hunter
22 November 2025While the article presents a compelling clinical narrative, it is critically deficient in acknowledging the structural barriers to clozapine access in underserved populations. The implicit assumption that patients possess the socioeconomic capital to comply with biweekly hematological monitoring is not merely optimistic-it is ethically negligent. Furthermore, the omission of cost disparities across U.S. states constitutes a material omission in a public health context.
Hannah Machiorlete
23 November 2025Ugh I tried clozapine. The weight gain was insane. I gained 60 lbs in 4 months. My boyfriend left. My therapist said ‘it’s not the drug, it’s the trauma’-like that helps when you can’t fit into your jeans. And don’t even get me started on the drooling. I had to sleep with a towel under my head. I’d rather hear the voices than wake up soaked.
Bette Rivas
25 November 2025For anyone considering clozapine: it’s not a magic bullet, but it’s the most evidence-based option for treatment-resistant schizophrenia. The key is early referral. Many clinicians wait too long to bring it up, often due to fear of liability or administrative burden. But studies show that delaying clozapine beyond 2 failed trials increases relapse risk by 40%. Also, side effects like sialorrhea can be managed with glycopyrrolate or even chewing gum. And yes, the blood work is a hassle-but it’s non-negotiable. Your life literally depends on it.
prasad gali
25 November 2025From a pharmacokinetic standpoint, clozapine’s polypharmacological profile-particularly its high affinity for 5-HT2A, D4, M1, and H1 receptors-renders it uniquely efficacious in modulating the cortico-limbic dysregulation characteristic of treatment-resistant psychosis. Other antipsychotics exhibit monoaminergic selectivity, which explains their limited impact on negative and cognitive domains. The agranulocytosis risk, while real, is mitigated through rigorous neutrophil monitoring protocols compliant with FDA and EMA guidelines. This is not a drug of last resort-it is the gold standard for neurobiological refractoriness.
Paige Basford
27 November 2025So I’ve been on clozapine for 3 years. I still get tired. I still have to go to the lab. But I made it to my sister’s wedding. I danced. I cried. I remembered what joy felt like. I used to think I was broken beyond repair. Turns out, I just needed the right key. And yeah, it’s messy. But so is life. I’m not perfect. I’m not ‘fixed.’ But I’m here. And that’s enough.
Ankita Sinha
29 November 2025Can we talk about how no one ever tells you that clozapine makes you crave peanut butter? Like, nonstop. I ate 3 jars in a week. My doctor laughed and said it’s the histamine blockade messing with appetite regulation. But honestly? I don’t care. If peanut butter is the price of hearing my own thoughts again, I’ll eat it till I’m 100. Also-has anyone else noticed clozapine makes you weirdly good at crossword puzzles? I solved a Sunday puzzle in 12 minutes. Weird. Cool. Thank you, brain.
Kenneth Meyer
30 November 2025There’s a quiet dignity in taking clozapine. It’s not about winning. It’s about showing up. Every week. For the blood draw. For the fatigue. For the stigma. You don’t get applause. You don’t get a medal. But you get to be present. To hold your child’s hand. To watch the sunset without fear. That’s not a miracle. That’s medicine doing its quiet, stubborn job. Maybe that’s all we ever really ask for: to be here, without being hunted by our own minds.
Lauren Hale
1 December 2025To the person who said they couldn’t afford blood tests: I’m so sorry you’re struggling. There are nonprofit programs and hospital financial aid options. I’ve helped 12 people navigate this. DM me if you need help finding resources. You don’t have to do this alone. And if you’re scared to talk to your doctor? Write it down. Send it as a message. They’ve seen it all. They want you to live.
Jonathan Gabriel
2 December 2025Wait… so clozapine works better than other drugs… but we don’t use it first because it’s ‘too risky’? Sounds like we’re prioritizing paperwork over people. Also, why does no one ever mention that clozapine makes you smell like faint cinnamon? I asked my pharmacist. She said it’s the metabolites. Weird. But I’ll take cinnamon over hallucinations any day.
Don Angel
4 December 2025Just one thing: if you’re on clozapine, please-please-don’t skip a blood test. I lost a friend. He missed one. He thought he’d be fine. He wasn’t. He was 28. Don’t be the next story.