Every year, thousands of patients in hospitals suffer preventable harm because of medication errors. Most of these mistakes don’t come from careless staff-they come from systems that don’t catch simple, high-risk mistakes before they happen. The biggest danger? High-alert medications. These aren’t just any drugs. They’re the ones that can kill a patient in minutes if given wrong-even if the dose is off by just a tenth of a milliliter. And yet, many healthcare workers still don’t know which ones truly require a second set of eyes before they’re given.
What Makes a Medication "High-Alert"?
A high-alert medication isn’t defined by how often it’s used, but by how much damage it can do when something goes wrong. The Institute for Safe Medication Practices (ISMP) first listed these drugs back in 2001, and they update the list every two years. The latest version, released in January 2024, includes 19 categories of medications that demand extra safeguards.These aren’t drugs you’d expect to be dangerous. Some look harmless-like saline or potassium-but in concentrated forms, they’re lethal. A single wrong IV push of potassium chloride can stop a heart. An overdose of insulin can send a patient into a coma. A misprogrammed infusion pump for heparin can cause internal bleeding. These aren’t theoretical risks. They happen every day in hospitals across the country.
The key isn’t that these drugs are used often-it’s that their margin for error is razor-thin. That’s why a simple typo, a misread label, or a rushed check can turn into a tragedy. And that’s why independent double checks exist: to catch those mistakes before the medication reaches the patient.
Which Medications Absolutely Require a Double Check?
Not every high-alert drug needs the same level of scrutiny. But some are non-negotiable. Here’s what most major healthcare systems in the U.S. and Australia now require an independent double check for:- IV insulin (both infusions and bolus doses)
- Potassium chloride concentrate (1 mEq/mL and higher)
- Potassium phosphate concentrate (1 mEq/mL and higher)
- IV heparin (including flushes over 100 units/mL)
- Neuromuscular blocking agents (like rocuronium or succinylcholine)
- Chemotherapeutic agents (all types, all routes)
- Injectable narcotic patient-controlled analgesia (PCA)
- Total parenteral nutrition (TPN) and lipid infusions
- Direct thrombin inhibitors (argatroban, bivalirudin)
- Continuous renal replacement therapy (CRRT) solutions (like Prismasol)
- All controlled substances (especially IV opioids like fentanyl or morphine)
Some institutions, like the Veterans Health Administration (VHA), require double checks for all high-alert medications. Others, like Providence Health System, limit it to the most dangerous ones. The difference? It comes down to risk assessment-not tradition.
The Real Meaning of "Independent Double Check"
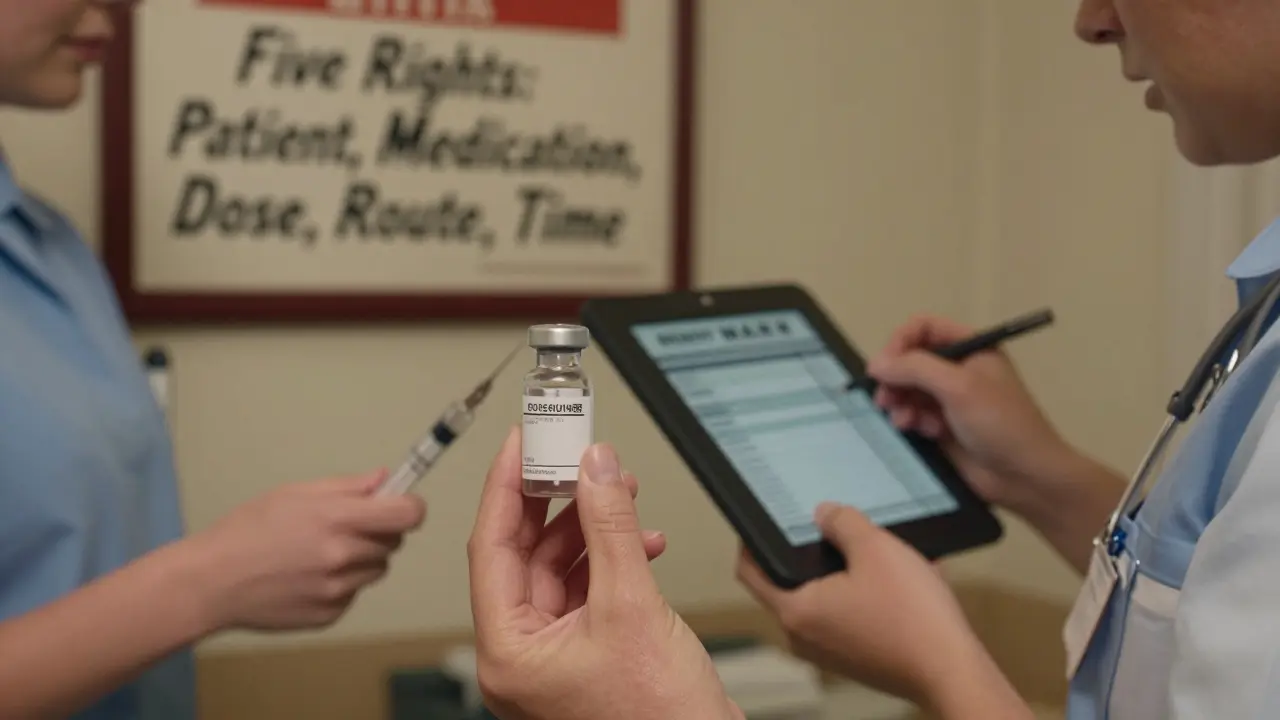
Here’s where most things go wrong. A "double check" isn’t just two people looking at the same thing at the same time. That’s not a double check-that’s a group think. The only kind that works is an independent double check.According to VHA Directive 1195 (updated October 2024), an independent double check means:
- Two licensed clinicians work alone, apart from each other.
- Each verifies all five rights: right patient, right medication, right dose, right route, right time.
- They don’t discuss what they’re seeing until after they’ve each completed their own check.
- They compare results only after both have independently verified everything.
- Both sign off electronically in the MAR (medication administration record).
Why does independence matter? Because if one person says, "I think it’s 10 units," the other might unconsciously look for confirmation instead of looking for error. That’s confirmation bias-and it’s why 68% of double checks that fail are done together, not independently.
One ICU nurse in Sydney told me she caught a 10-fold overdose of heparin last month because the second nurse, working alone, noticed the pump was set to 20 units/hour instead of 2. The first nurse had assumed it was right because "it looked normal." That’s the exact failure mode independent checks are designed to prevent.

What to Check During a Double Check
A proper double check isn’t a quick nod. It’s a full audit. Here’s what you must verify for every high-alert medication:- Patient identity: Two unique identifiers-name and date of birth, not room number or wristband color.
- Medication name: Read the label out loud. Match it to the eMAR. Don’t assume because it’s in the same drawer.
- Dose and strength: Calculate it yourself. Don’t rely on the pharmacy label. If it’s 10 mEq of KCl, confirm the vial isn’t 20 mEq.
- Route: Is this supposed to be IV? Or is it a tablet? Mixing routes kills.
- Time and frequency: Is this a one-time dose? Or a continuous infusion? Does the schedule match the order?
- Pump settings: For infusions, verify rate, volume, concentration, and duration. Smart pumps help-but they’re not foolproof.
At Johns Hopkins, they reduced heparin errors by 82% after they added a checklist to their double-check protocol. Nurses now carry laminated cards listing exactly what to verify. Simple. Repeatable. Effective.
Why So Many Double Checks Fail
The biggest myth? That double checks are foolproof. They’re not. If done poorly, they’re barely better than no check at all.ECRI Institute found that when double checks are done correctly, they prevent 95% of errors. But when done incorrectly-like when nurses check together, rush through it, or skip steps-they only catch 40% of mistakes. That’s worse than having no safety net at all.
Here’s what goes wrong in real life:
- Simultaneous checking: Two nurses standing side by side, one says "10 units," the other nods. No real verification.
- Time pressure: During a code, nurses skip checks because "it’s urgent." But 68% of fatal errors happen during emergencies.
- Unclear protocols: If your hospital doesn’t say exactly what to check, nurses guess. And guessing kills.
- Documentation fatigue: Nurses skip signing off because the system is clunky. But if it’s not documented, it didn’t happen.
- Staff shortages: No second nurse available? That’s not an excuse-it’s a system failure.
A 2023 survey of 1,200 nurses found that 78% believed all high-alert meds should require double checks. But ISMP says that’s the wrong approach. Too many checks mean they become routine-and routine means careless.
The Smart Way Forward
The future isn’t more double checks. It’s smarter ones.Leading hospitals are shifting from blanket rules to targeted safety. Here’s what works:
- Use technology: Smart pumps with dose error reduction systems (DERS) automatically flag unsafe doses. When paired with double checks for only the highest-risk drugs, error rates drop 63%.
- Train properly: Cleveland Clinic requires a 2-hour competency session before anyone can perform double checks. Annual refreshers are mandatory. Pass rate: 95%.
- Build time in: Mayo Clinic includes double-check time in staffing models. No more "I don’t have time." It’s part of the job.
- Use eMAR with dual signatures: If the system won’t let you sign off without two people, you can’t skip it.
- Review errors monthly: Look at near-misses. What went wrong? Adjust your protocol.
At the Royal Melbourne Hospital, they cut insulin errors by 75% in 12 months by reducing double checks to just three drugs-insulin, heparin, and potassium-and making sure every check was truly independent. Staff resistance dropped once they saw fewer mistakes and less paperwork.
What You Can Do Today
You don’t need a hospital-wide overhaul to make a difference. Start here:- Know your list. Ask your pharmacy or safety officer for the current high-alert medication list at your facility.
- Practice independence. Next time you double check, go to a different corner of the unit. Don’t talk until you’re both done.
- Speak up. If you see someone doing a "simultaneous check," say: "Can we do this independently? I want to make sure we catch everything."
- Check your eMAR. Is dual signing required? If not, push for it.
- Report near-misses. Even if no one got hurt, if a mistake almost happened, document it. That’s how systems improve.
Medication safety isn’t about blame. It’s about building layers of protection so that when one fails, another catches it. The double check is one of those layers. But only if it’s done right.
Don’t just check the box. Check the patient.”
What are the most dangerous high-alert medications that require a double check?
The most dangerous medications requiring independent double checks include IV insulin, concentrated potassium chloride (1 mEq/mL and above), IV heparin (especially flushes over 100 units/mL), neuromuscular blocking agents like rocuronium, chemotherapy drugs, and injectable narcotic PCA pumps. These drugs have a narrow therapeutic window-small errors can lead to cardiac arrest, respiratory failure, or death. Even a 10-fold overdose of insulin can send a patient into a coma.
Is a double check always necessary for high-alert medications?
No. The Institute for Safe Medication Practices (ISMP) advises against universal double checks. Instead, they recommend using them only for the highest-risk medications and situations-like IV insulin, heparin infusions, and pediatric chemotherapy. Overusing double checks leads to complacency. The goal isn’t to check everything-it’s to protect against the errors that could kill.
What’s the difference between a simultaneous check and an independent double check?
A simultaneous check is when two people look at the medication together, often talking as they go. That’s not independent-it’s groupthink. An independent double check means two licensed clinicians verify the medication alone, apart from each other, then compare results only after both have completed their own verification. This prevents confirmation bias and catches hidden errors.
Why do double checks sometimes fail to prevent errors?
Double checks fail when they’re rushed, done together, or poorly trained. Studies show that when nurses perform checks side-by-side, error detection drops to just 32%. Other causes include unclear protocols, lack of time, staff shortages, and skipping documentation. If the process isn’t standardized and respected, it becomes a formality-not a safety net.
Can technology replace the need for double checks?
Technology like smart pumps with dose error reduction systems (DERS) and electronic MARs with dual signatures can reduce errors significantly-but they don’t eliminate the need for human verification. The most effective systems combine technology with targeted double checks. For example, smart pumps flag wrong doses, but a nurse still verifies the patient and drug name. Human judgment remains essential for complex cases like chemotherapy or unstable patients.
What should I do if there’s no second nurse available during an emergency?
In emergencies, double checks are often delayed-but never skipped. If no second licensed clinician is available, use a second set of eyes: a pharmacist, a tech with training, or even a second provider. Document the reason for the delay. After the emergency, complete the double check retroactively and report the gap. Hospitals should have backup protocols for staffing shortages-like rapid-response teams trained in medication safety.
How can I tell if my facility’s double-check protocol is effective?
Look at your error rates. If high-alert medication errors have dropped since the protocol started, it’s working. Also, audit a sample of double checks-do nurses verify all five rights? Are they truly independent? Are signatures required in the eMAR? Ask staff: Do they feel safe speaking up if something looks wrong? If the answer is yes, your system is strong.
Next Steps for Healthcare Teams
If you’re in a leadership role, start by auditing your current double-check process. How many medications require it? Are the steps clearly written? Are staff trained? Are errors being tracked? If you’re a frontline clinician, don’t wait for policy changes-start practicing true independence today. One honest double check could be the difference between a patient going home-or not.Medication safety isn’t about perfection. It’s about persistence. And every time you take that extra 90 seconds to verify properly, you’re not just following protocol-you’re saving a life.







Dan Padgett
16 December 2025Man, this post hit different. I’ve seen nurses do double checks like they’re rushing through a grocery list-glance at the label, nod, sign. One time, I watched a guy give 10x the potassium dose because the second nurse just said, ‘Yeah, that looks right.’ No calculation. No reading the vial. Just vibes. We’re not saving lives with good intentions. We’re saving them with discipline.
Kayleigh Campbell
16 December 2025Let’s be real-double checks are the hospital equivalent of wearing seatbelts. You don’t do it because you think you’ll crash, you do it because you know you might. And yet, we treat it like a chore. I’ve seen people do ‘independent’ checks while standing shoulder-to-shoulder, whispering ‘is this 5 or 10?’ like it’s a game of hide-and-seek. If your protocol doesn’t force physical separation, it’s theater.
Cassandra Collins
17 December 2025Wait… so you’re telling me the system is designed to kill people on purpose? I mean, why else would they let nurses skip checks during emergencies? I’ve heard stories-pharmacies get hacked, pumps get reprogrammed by interns, and the ‘second nurse’ is just the charge nurse who’s also doing 3 codes and a code blue. This isn’t safety. This is a death lottery with a clipboard.
Ron Williams
18 December 2025As someone who’s worked in rural India and now in a NYC ER, I can say this: the problem isn’t the meds-it’s the culture. In Mumbai, we did double checks with a chai break in between. Two people, one pot, no rush. Here? We’re told to ‘move fast or get out.’ No wonder people burn out. Safety isn’t a checklist. It’s a rhythm. And we’ve lost the beat.
Aditya Kumar
18 December 2025Too much text. Just tell me the list.
Kim Hines
19 December 2025I used to skip the independent part because I trusted my partner. Then I saw a 72-year-old go into cardiac arrest because we both missed the 10-fold heparin dose. We were ‘both checking.’ We were wrong. Now I walk to the other end of the unit. I don’t say a word until I’m done. It’s weird. It’s slow. It’s the only thing that keeps me sleeping at night.
Randolph Rickman
20 December 2025YES. This. I work in oncology. Chemo errors are silent killers. We started using laminated checklists and mandatory dual eMAR signatures-and our near-misses dropped 70% in 6 months. It’s not magic. It’s just doing the damn thing right. Stop treating safety like a suggestion. It’s your license to practice. If you’re tired of the checklist, maybe you’re tired of being a nurse.
Andrew Sychev
20 December 2025Look, I get it. Double checks are annoying. But if you think I’m gonna let some intern push a vial of potassium without me physically walking over, reading the label out loud, and then comparing it to the eMAR with my own eyes-you’re not working with me. I don’t care if you’re my best friend. If you’re not independent, you’re a liability. And I will call you out in front of everyone. Because one mistake, and you don’t just lose your job-you lose someone’s mom.
Billy Poling
22 December 2025It is imperative to underscore the necessity of institutional adherence to standardized, evidence-based protocols governing the administration of high-alert pharmaceutical agents. The absence of uniform policy enforcement across clinical departments constitutes a systemic vulnerability that directly contravenes the principles of patient-centered care as articulated by the Joint Commission and the World Health Organization’s Global Patient Safety Action Plan. Furthermore, the reliance on human verification in high-stress environments, absent technological augmentation such as barcode medication administration (BCMA) and real-time clinical decision support (CDS) integration, represents an antiquated paradigm that is statistically untenable in the context of modern healthcare delivery systems.
Arun ana
23 December 2025Big respect to everyone sharing their stories. I’ve been in hospitals where the double check was just a formality… and others where it felt like a sacred ritual. The difference? Leadership. When the charge nurse actually stops and watches, when the pharmacy sends someone to shadow, when the hospital tracks near-misses like gold-then people care. It’s not about rules. It’s about showing up for each other. 🙏