Thyroid disorders: Symptoms, tests, and treatment options
Thyroid disorders affect how your body uses energy and can change weight, mood, and energy levels fast. This page gives clear, practical info on common thyroid problems, how they are tested, and treatment choices you can talk about with your doctor.
Hypothyroidism means the thyroid is underactive. Common signs are weight gain, cold intolerance, fatigue, slow heart rate, dry skin, hair loss, and heavy periods. Hyperthyroidism is the opposite: weight loss, heat intolerance, fast heartbeat, anxiety, tremors, and loose stools. Both can be subtle, so check tests if you have persistent symptoms.
The basic tests are TSH and free T4. TSH tells your pituitary response; free T4 shows available thyroid hormone. If results are unclear, doctors may order free T3, thyroid peroxidase antibodies (TPO), or radioactive uptake scans. In many cases blood tests plus a clinical exam are enough to start treatment.
Most people with an underactive thyroid take levothyroxine (brand names include Synthroid). It restores T4 levels and is usually taken once daily on an empty stomach, 30–60 minutes before breakfast. Don’t take it with calcium, iron, or antacids — these reduce absorption. If you still feel unwell after a correct dose and normal labs, ask your doctor about combination therapy (T4+T3) or desiccated thyroid extract. Those are options but need careful monitoring.
For overactive thyroid, treatments include antithyroid pills (methimazole or propylthiouracil), radioactive iodine, or sometimes surgery. Which one fits depends on age, severity, pregnancy plans, and other health issues. Your doctor will explain risks and follow-up.
Lifestyle choices help but don’t replace medicine. Keep consistent timing for meds, avoid large amounts of soy or high-calcium meals right after dosing, and manage stress and sleep. Ensure adequate iodine if you live where deficiency is common, but don’t take high-dose iodine supplements without medical advice. Selenium supplements may help in autoimmune thyroiditis for some people, but check with your clinician first.
Monitoring matters. After starting or changing a dose, labs are checked every 6–8 weeks until stable. Once stable, yearly TSH testing is common, more often in pregnancy or if symptoms change. Bring a list of your medicines and supplements to appointments so interactions don’t get missed.
If you have sudden neck pain, racing heart, extreme weakness, or fainting, seek immediate care. For most other thyroid concerns, book an appointment with your primary care doctor or an endocrinologist.
Explore related pieces on this site about Synthroid alternatives, testing tips, and medication safety. Read those articles to learn specific pros and cons before deciding with your doctor.
Pregnancy and planning pregnancy change targets: doctors aim for a lower TSH and often increase levothyroxine dose early in pregnancy; tell your provider if you are pregnant or trying. Older adults may need lower doses and closer monitoring because heart issues can limit how much hormone is safe. Travel with meds in original bottle, keep a copy of your prescriptions, and avoid switching brands without medical advice. If you use supplements, list doses so your clinician can adjust therapy safely. Ask questions often.
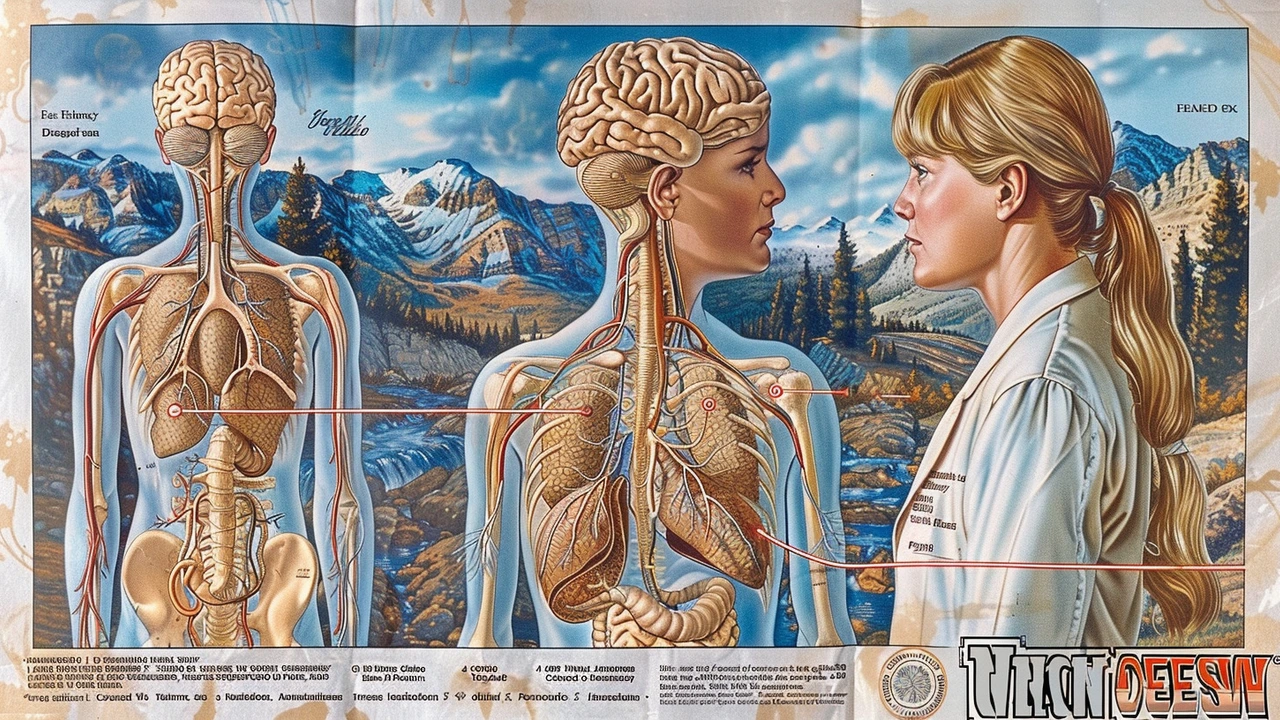
Understanding the Link Between Central Cranial Diabetes Insipidus and Thyroid Disorders
This article explores the connection between central cranial diabetes insipidus and thyroid disorders. It delves into how these conditions interplay, affect the body, and what symptoms to watch for. Practical tips and interesting facts are provided to help those affected manage their health more effectively.
Health and WellnessLatest Posts
Tags
- online pharmacy
- medication safety
- generic drugs
- medication
- dietary supplement
- side effects
- online pharmacy UK
- drug interactions
- mental health
- impact
- online pharmacies
- statin side effects
- dosage
- generic vs brand
- pediatric antibiotics
- antibiotic side effects
- skin health
- health
- pain relief
- dietary supplements