Male Infections: Causes, Symptoms, and Treatment Options
When dealing with Male Infections, infections that primarily affect men's reproductive and urinary systems. Also known as men's infections, it can arise from bacteria, viruses, fungi or parasites and often needs prompt attention to avoid complications.
One of the most frequent complaints is Urinary Tract Infection, an infection of the bladder, urethra or kidneys that causes burning, frequent urination and sometimes fever. Though women experience UTIs more often, men can develop them after prostate procedures, catheter use or when the urinary flow is obstructed. Early diagnosis usually involves a simple urine test, and treatment typically relies on a short course of antibiotics tailored to the pathogen.
Another major group is Sexually Transmitted Infection, infections passed through sexual contact, including chlamydia, gonorrhea, syphilis and human papillomavirus. These conditions often start with mild discomfort or no symptoms at all, which is why regular screening is crucial. Untreated STIs can lead to infertility, chronic pain or systemic spread, so modern guidelines recommend a combination of antibiotics, antivirals, or vaccine‑based prevention where available.
Prostatitis, the inflammation of the prostate gland, represents a third common scenario. It can be bacterial—either acute, with sudden fever and painful urination, or chronic, with lingering pelvic pain and urinary issues. Non‑bacterial prostatitis may stem from nerve irritation or autoimmune factors. Diagnosis usually combines a digital exam, urine analysis and sometimes an ultrasound, while treatment ranges from a full antibiotic regimen for bacterial forms to anti‑inflammatory drugs and lifestyle adjustments for chronic cases.
Fungal infections, often overlooked, also affect men, especially athletes and those with compromised immunity. Fungal Infection, a skin or mucosal infection caused by organisms like Candida or dermatophytes, can appear as athlete's foot, jock itch or oral thrush. These conditions thrive in warm, moist environments, so proper foot hygiene, breathable clothing and prompt antifungal treatment are key. In severe cases, oral antifungals may be prescribed.
How These Infections Interact and What to Watch For
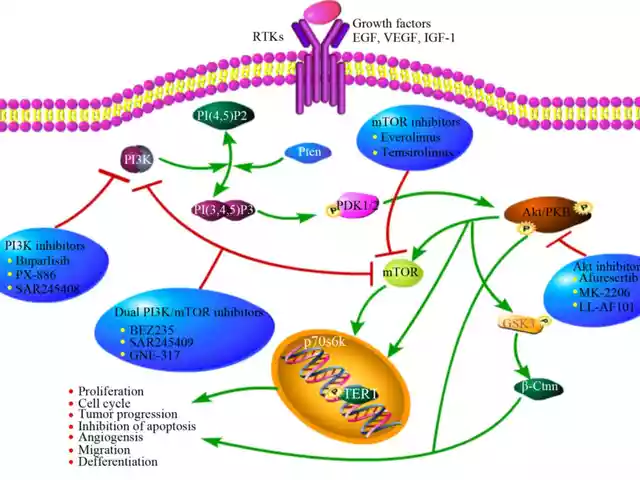
Male infections often overlap. For example, a persistent urinary tract infection can irritate the prostate, turning a simple UTI into prostatitis. Likewise, an untreated sexually transmitted infection can spread to the urinary tract or cause secondary fungal growth due to immune suppression. HIV, a virus that weakens the immune system, amplifies the risk of all these infections, making early testing and consistent antiviral therapy essential.
Key attributes to keep in mind include the pathogen type (bacterial, viral, fungal), typical symptoms (pain, discharge, itching, fever), diagnostic methods (urine culture, swab PCR, imaging) and effective treatments (antibiotics, antivirals, antifungals, lifestyle changes). Understanding these attributes helps you spot red flags early and choose the right medical help.
Practical steps you can take right now are simple: stay hydrated, practice safe sex, keep the genital area clean and dry, and don’t ignore persistent discomfort. If you notice any of the warning signs—burning during urination, unusual discharge, pelvic pain, or skin irritation—schedule a visit with a healthcare provider. Early intervention not only speeds recovery but also prevents long‑term damage.
Below you’ll find a curated collection of articles that dive deeper into each of these topics, from footgear that eases muscle stiffness to the latest on HIV treatment, antifungal research and more. Use them as a roadmap to understand symptoms, explore treatment options, and stay ahead of potential complications.
Secnidazole for Men: How to Treat Male Trichomoniasis & Other Infections
Learn how secnidazole treats male trichomoniasis, giardiasis, and amoebiasis, including dosage, side effects, drug interactions, and practical FAQs for men's health.
MedicationsLatest Posts
Tags
- online pharmacy
- medication safety
- generic drugs
- medication
- dietary supplement
- side effects
- online pharmacy UK
- drug interactions
- mental health
- impact
- online pharmacies
- statin side effects
- dosage
- generic vs brand
- pediatric antibiotics
- antibiotic side effects
- skin health
- health
- pain relief
- dietary supplements