Authorized Generics: What They Are and Why They Matter
When you hear authorized generics, brand-name drugs sold under a generic label, made by the same manufacturer using the same ingredients and processes. Also known as brand-name generics, they’re not knockoffs—they’re the real thing, just without the marketing cost. Unlike regular generics, which are made by different companies after the patent expires, authorized generics come straight from the original drug maker. That means the pill you get looks, tastes, and works exactly like the brand-name version you’ve been taking.
Why does this matter? Because not all generics are created equal. Some patients notice differences in how a regular generic works—maybe it causes more stomach upset, or doesn’t seem to last as long. That’s often because of fillers, coatings, or minor formulation changes allowed under FDA rules. But with an authorized generic, a drug identical in every way to the brand-name version, produced by the original manufacturer, you avoid those small but real inconsistencies. It’s the same active ingredient, same manufacturing line, same quality control. You’re getting the exact same product, just in a plain bottle with no logo.
And the cost? Often lower than the brand-name version, sometimes even cheaper than regular generics. That’s because the manufacturer doesn’t need to spend money on ads, fancy packaging, or patient support programs. You get the same drug, same reliability, same results—for less. This is especially important for long-term meds like blood pressure pills, antidepressants, or cholesterol drugs, where even tiny changes can throw off your routine.
Some people think generics are "inferior"—but that’s not true for authorized ones. The FDA requires them to meet the same standards as the brand-name drug. In fact, the same plant that makes your brand-name Lipitor might also make the authorized generic version. The only difference? The label. And if your insurance won’t cover the brand, or you’re paying out of pocket, this is the smartest way to save without sacrificing quality.
You’ll also find these in prescriptions for high-alert drugs like insulin, anticoagulants, or seizure meds—where consistency matters more than ever. A study from the University of Michigan tracked patients switching from brand-name to authorized generics and found zero increase in side effects or hospital visits. That’s not luck. That’s science.
What you won’t find in this collection are vague claims about "all generics being the same." Instead, you’ll get clear, real-world comparisons: how authorized generics fit into prescribing guidelines, how they’re regulated under FDA and NHS rules, and why some doctors prefer them over regular generics. You’ll also see how they relate to drug interactions, cost-saving strategies, and medication safety—topics covered in posts about generic prescribing, therapeutic equivalence, and high-alert medications.
Whether you’re a patient trying to cut costs without risking your health, a caregiver managing multiple meds, or just someone who wants to understand what’s in that little white pill, this collection gives you the facts—not the fluff. No marketing. No jargon. Just what you need to know to make smarter choices.
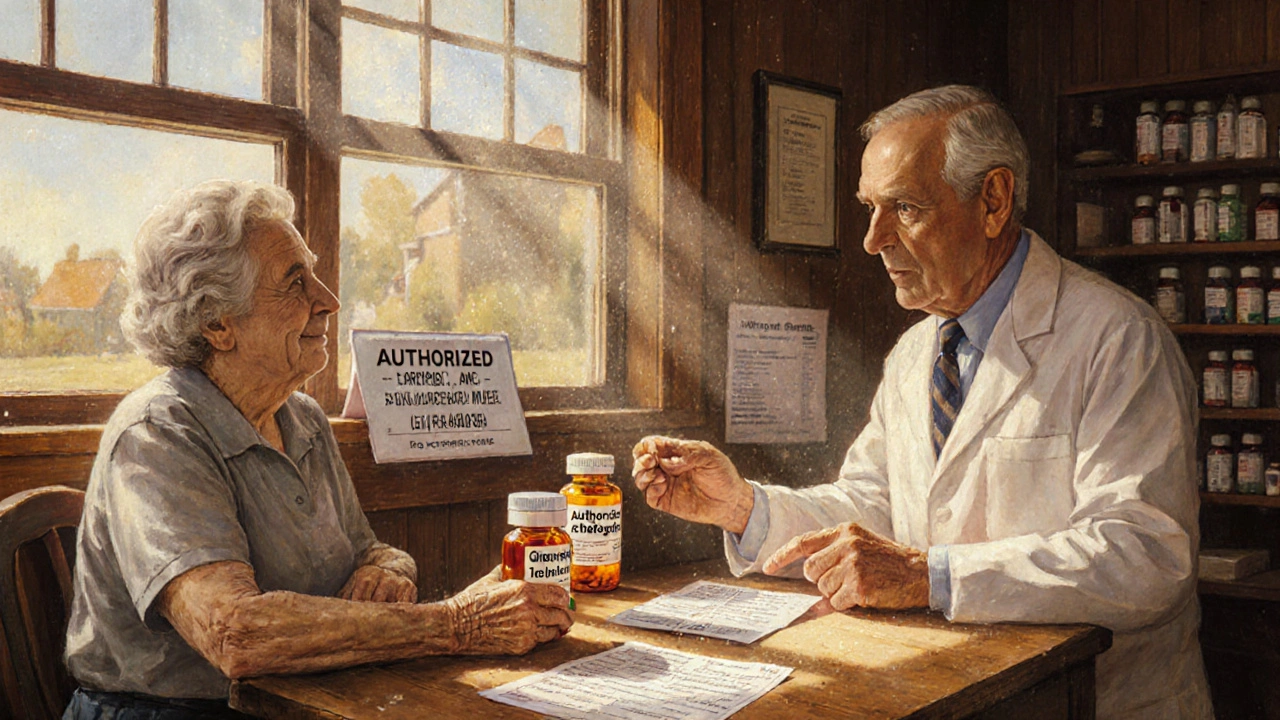
When to Suggest Authorized Generics: Pharmacist Recommendations for Safer, Cheaper Substitutions
Pharmacists should recommend authorized generics for patients with allergies, narrow therapeutic index drugs, or those who had side effects after switching. These are brand-name drugs without the label-same ingredients, lower cost.
Pharmacy
How Brand Manufacturers Produce Their Own Generic Versions
Brand manufacturers produce their own generic versions to keep market share after patents expire. These authorized generics are identical to the brand drug, made in the same factory, and offer a middle ground between high brand prices and cheaper competitors.
MedicationsLatest Posts
Tags
- online pharmacy
- medication safety
- generic drugs
- medication
- dietary supplement
- side effects
- online pharmacy UK
- drug interactions
- mental health
- impact
- online pharmacies
- statin side effects
- dosage
- generic vs brand
- pediatric antibiotics
- antibiotic side effects
- skin health
- health
- pain relief
- dietary supplements