Dual Antiplatelet Therapy GI Bleed Risk Assessment
Assess Your GI Bleeding Risk
This tool helps determine if you need a proton pump inhibitor (PPI) while on antiplatelet therapy and which PPI is safe for you.
When you’re on dual antiplatelet therapy - usually aspirin plus clopidogrel, prasugrel, or ticagrelor - your blood doesn’t clot as easily. That’s good for preventing heart attacks and strokes. But it also means your stomach is more vulnerable. Up to 1 in 3 people on this combo will develop a gastrointestinal bleed within the first year. And for some, it’s life-threatening.
The solution isn’t to stop the blood thinners. It’s to protect the stomach. That’s where proton pump inhibitors (PPIs) come in. Used correctly, they cut the risk of serious GI bleeding by a third to nearly 40%. But not all PPIs are created equal. And not everyone needs them. Getting this right matters - because the wrong choice can undo the heart protection you’re counting on.
Why Antiplatelets Hurt Your Stomach
Aspirin and other antiplatelet drugs don’t just thin your blood. They also weaken the lining of your stomach and upper intestine. They block protective prostaglandins, which normally help your stomach repair itself and maintain a healthy acid barrier. Without them, even normal stomach acid can start eating away at your tissue.
Studies show that people on aspirin alone have 2 to 4 times the risk of GI bleeding compared to those not taking it. Add a second antiplatelet like clopidogrel, and that risk jumps another 30-50%. The highest danger window? The first 30 days after starting treatment. Nearly three-quarters of serious bleeds happen during this time.
That’s why guidelines now say: if you’re on dual therapy, you’re at higher risk - and you need protection. But here’s the catch: not all PPIs are safe to take with all antiplatelets.
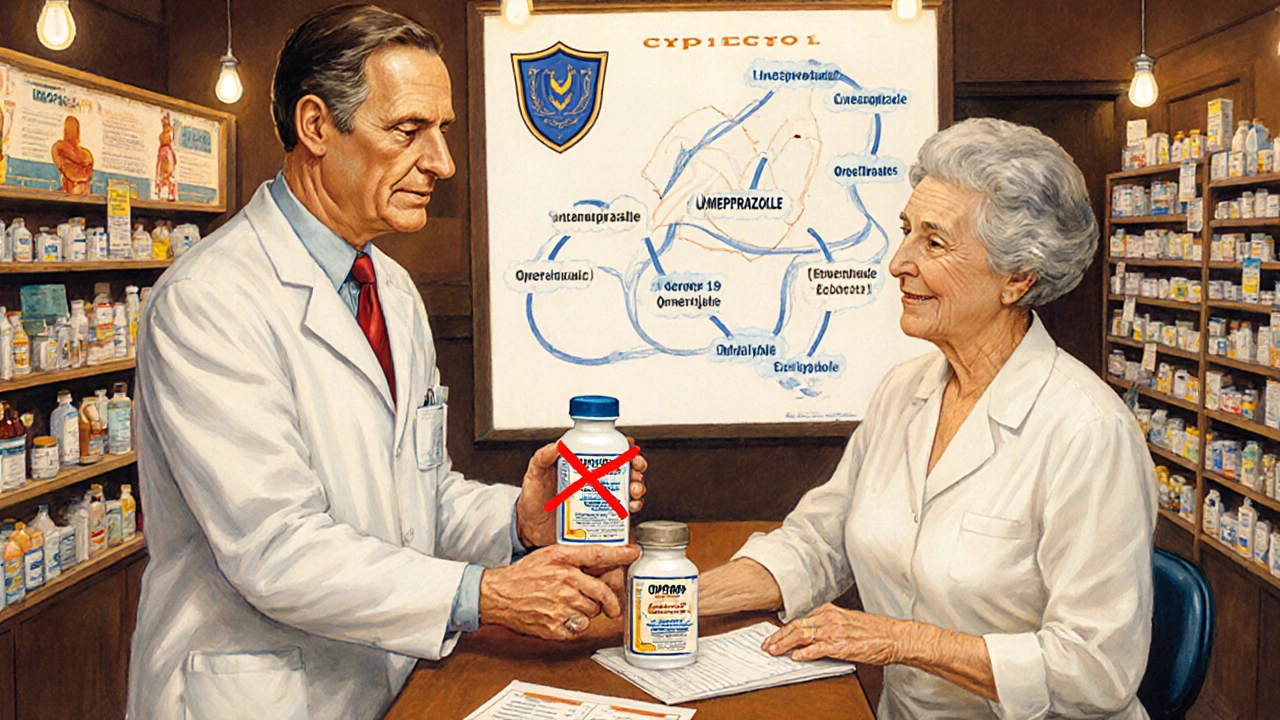
Which PPIs Work Best - and Which Can Hurt
PPIs like omeprazole, esomeprazole, and pantoprazole shut down stomach acid production by blocking the proton pump in stomach cells. That’s great for healing ulcers and preventing bleeds. But omeprazole has a hidden problem: it interferes with clopidogrel.
Clopidogrel needs to be activated by an enzyme called CYP2C19. Omeprazole blocks that enzyme. Studies show this cuts clopidogrel’s antiplatelet effect by up to 30%. That means your blood isn’t as thin as it should be - and your risk of a heart attack or stent clot goes up. One 2010 meta-analysis found this interaction could increase cardiovascular events by 27%.
That’s why experts now say: avoid omeprazole if you’re on clopidogrel.
Instead, choose pantoprazole or esomeprazole. Both are just as good at protecting your stomach - but they barely touch CYP2C19. In fact, pantoprazole reduces clopidogrel’s effect by less than 15%. Esomeprazole? Almost none. And if you’re on ticagrelor or prasugrel? Those drugs don’t rely on CYP2C19 at all. So you can safely use any PPI, including omeprazole.
How Much Do You Really Need?
Not everyone on antiplatelets needs a PPI. The key is risk. The 2023 European Society of Cardiology guidelines say: give a PPI if you have two or more of these risk factors:
- History of stomach bleeding or ulcers
- Age 65 or older
- Taking steroids or NSAIDs (like ibuprofen or naproxen)
- On blood thinners like warfarin or apixaban
If you’re 52, healthy, and only on aspirin? You probably don’t need one. But if you’re 72, on aspirin and clopidogrel, and take daily ibuprofen for arthritis? You absolutely do.
Here’s the problem: too many people get PPIs they don’t need. A 2022 study found 35-45% of prescriptions for DAPT patients were inappropriate. That’s a lot of unnecessary pills. And they come with their own risks.
The Hidden Risks of Long-Term PPI Use
PPIs are safe for short-term use - but taking them for years without reason can cause real harm.
- Higher risk of C. difficile infection: 0.5% increase in absolute risk
- Increased chance of pneumonia: 0.8% higher risk
- Higher risk of chronic kidney disease: hazard ratio of 1.20
- Potential link to bone fractures with long-term, high-dose use
Even the FDA has issued warnings. And new research in 2024 suggested a possible connection between long-term PPI use and dementia - though a 2025 Mendelian randomization study found no causal link. The evidence isn’t settled, but the pattern is clear: if you don’t need it, don’t take it.
That’s why most guidelines recommend PPIs for 6-12 months after starting DAPT - unless you’re still at high risk. After that, reassess. Can you stop it? Or do you need to keep going?
What About H2 Blockers? Are They an Alternative?
Some people ask: why not use famotidine or ranitidine instead? They’re cheaper and don’t interact with clopidogrel.
But here’s the data: they’re not as good. A 2017 JAMA meta-analysis showed PPIs reduced upper GI bleeding by 60%. H2 blockers? Only 30%. The absolute difference? 1.8% vs. 0.9%. That means for every 55 people you treat with a PPI instead of an H2 blocker, you prevent one major bleed.
Bottom line: if you need protection, go with a PPI. If you don’t need it, don’t take either.
Dosing and Timing: When to Start and How Much
Start the PPI on day one - not after the first stomach ache. The first 30 days are the most dangerous. Waiting until you have symptoms is too late.
Standard doses:
- Pantoprazole: 40 mg once daily
- Esomeprazole: 20-40 mg once daily
- Omeprazole: 20-40 mg once daily - only if not on clopidogrel
Take it 30 minutes before breakfast. That’s when your stomach’s proton pumps are most active. Taking it after eating reduces effectiveness.
Don’t double up. More isn’t better. High doses don’t offer extra protection - and they raise your risk of side effects.

What If You Can’t Afford or Access a PPI?
Generic pantoprazole costs under $5 a month in the U.S. and is available over the counter. Esomeprazole is slightly more expensive but still affordable. If cost is a barrier, talk to your pharmacist. Many drug manufacturers have patient assistance programs.
And if your doctor says you don’t need one - but you’re worried? Ask for a risk score. Use the AIMS65 or Glasgow-Blatchford score. These tools help turn guesswork into data. You deserve to know your real risk - not just be told to take a pill.
The Bigger Picture: Underused and Overused
Here’s the paradox: in Europe, 55-65% of DAPT patients get PPIs. In the U.S., it’s only 40-50%. But at the same time, nearly half of those prescriptions are for people who don’t need them.
That’s a system failing on both ends. Some patients are unprotected. Others are overmedicated.
The answer isn’t blanket rules. It’s personalized care. Use your history, your age, your other meds, your genetics - if you know them. A 2024 Mayo Clinic study found that people with certain CYP2C19 gene variants respond poorly to clopidogrel. For them, switching to ticagrelor and using any PPI might be the safest path.
The future is precision. But today, the best tool you have is simple: ask your doctor, “Am I at high risk for GI bleeding? And if so, which PPI is safest with my antiplatelet?”
What’s Coming Next
Researchers are working on better options. Vonoprazan, a new type of acid blocker called a potassium-competitive acid blocker, is under FDA review. It works faster, lasts longer, and doesn’t interfere with clopidogrel. Early trials show it’s as good as esomeprazole at preventing bleeds - without the interaction risk.
And the PRECISION-DAPT registry, launching in 2024, will track 15,000 patients to better define who truly benefits from long-term PPI use. We’re moving beyond one-size-fits-all.
For now, stick with what works. If you’re on aspirin and clopidogrel, ask for pantoprazole or esomeprazole. If you’re on ticagrelor or prasugrel, any PPI is fine. But if you’re low-risk? Don’t take one. And if you’ve been on one for years? Ask if you still need it.
Protecting your stomach doesn’t mean taking more pills. It means taking the right ones - at the right time - for the right reason.
Can I take omeprazole with clopidogrel?
No, it’s not recommended. Omeprazole blocks the enzyme (CYP2C19) your body needs to activate clopidogrel. This can reduce its effectiveness by up to 30%, increasing your risk of heart attack or stent clot. Use pantoprazole or esomeprazole instead. If you’re already on omeprazole, talk to your doctor about switching.
Do I need a PPI if I’m only on aspirin?
Only if you’re at high risk for GI bleeding - like if you’re over 65, have a history of ulcers, or take NSAIDs or steroids. If you’re young and healthy, the risk of bleeding from aspirin alone is low, and the risks of long-term PPI use may outweigh the benefits. Talk to your doctor about your personal risk score.
How long should I take a PPI with antiplatelets?
Most guidelines recommend 6 to 12 months - especially during the first year after a heart attack or stent, when bleeding risk is highest. After that, reassess. If you still have risk factors like age, NSAID use, or prior bleeding, you may need to continue. If not, consider stopping. Don’t stay on it longer than needed.
Are there natural alternatives to PPIs for stomach protection?
No. While diet, probiotics, and avoiding alcohol or NSAIDs can help reduce irritation, none have been shown to prevent serious GI bleeding caused by antiplatelet drugs. PPIs are the only proven, evidence-based protection. Don’t rely on supplements or lifestyle changes alone if you’re at high risk.
Can PPIs cause kidney damage?
Long-term use of PPIs is linked to a slightly higher risk of chronic kidney disease - with a hazard ratio of about 1.20. That means a 20% increased relative risk. But the absolute risk is still low. For most people, the benefit of preventing a life-threatening GI bleed outweighs this small risk - if the PPI is truly needed. Avoid unnecessary long-term use.






Tiffanie Doyle
28 October 2025I was on clopidogrel for a year after my stent and my doc gave me omeprazole... turns out that was a mistake. Switched to pantoprazole and no more stomach issues. Also, my heart feels way more stable now. 🙌
james landon
29 October 2025lol why are we all taking pills for pills? I just drink ginger tea and call it a day. My stomach’s fine.
Jenn Clark
30 October 2025This is such a clear breakdown. I’ve been on aspirin + clopidogrel since 2021 and my GI doc insisted on pantoprazole - I didn’t understand why until now. Thanks for explaining the CYP2C19 thing. So much better than just being told ‘take this’.
L Walker
31 October 2025PPIs are overprescribed, period. My GP gave me one after a single aspirin prescription. I stopped after two weeks. No bleeding. No drama. The system is broken. Also, H2 blockers are underrated. Just saying.
giri pranata
31 October 2025In India, we don’t even think about this stuff. People just take aspirin + omeprazole because it’s cheap and available. But now I see why that’s risky. Thanks for the clarity - gonna share this with my uncle who’s on dual therapy.
Stuart Rolland
1 November 2025I’ve been on ticagrelor for three years now, and honestly, I didn’t even know PPIs could interfere with clopidogrel until I read this. I take esomeprazole because my cardiologist said it’s safe, and honestly, I’ve never had a single stomach issue. But I’ve also seen friends on omeprazole who had silent bleeds - one ended up in ICU. So yeah, this isn’t just academic. It’s life or death. And the fact that so many docs still default to omeprazole? That’s terrifying. We need better education. Not just for patients, but for the people prescribing these drugs. I mean, if you’re not up to speed on CYP2C19 interactions, maybe you shouldn’t be managing DAPT patients at all.
Kent Anhari
2 November 2025I’m 58, on aspirin and clopidogrel, no other meds, no history of ulcers. My doctor said I don’t need a PPI. I asked for one anyway because I was scared. He looked at me like I was crazy. Then he ran my risk score - AIMS65 came back 0.5. Said I’m lower risk than my cat. So I didn’t take it. Still feel fine. Point is: ask for data, not fear.
Charlos Thompson
4 November 2025Oh wow, so the real problem isn’t GI bleeds - it’s that pharma doesn’t want you to know H2 blockers are cheaper and just as safe for low-risk folks. And now we’ve got a whole industry built around selling $200/month PPIs to people who don’t need them. Brilliant business model. #BigPharmaWins
Peter Feldges
5 November 2025I appreciate the depth of this post. However, I must note that while the CYP2C19 interaction is well-documented, recent meta-analyses (e.g., JAMA Cardiology 2023) suggest the clinical impact may be overstated in real-world populations with adherence monitoring. Also, the 2025 Mendelian randomization study on dementia, while reassuring, was observational - we still lack RCT data. Precision medicine is ideal, but population-level guidelines must account for variability in access, compliance, and genetic testing availability. I’m not dismissing the guidance - just urging nuance.
Richard Kang
5 November 2025I’M ON ASPIRIN AND CLOPIDOGREL AND I’VE BEEN TAKING OMEPRAZOLE FOR 5 YEARS AND I’M FINE!!! WHY IS EVERYONE SO SCARED?! MY DOCTOR SAID IT WAS FINE AND HE’S A CARDIOLOGIST!!! YOU PEOPLE ARE OVERANALYZING EVERYTHING!!!
Rohit Nair
5 November 2025I read this and thought about my dad in Delhi - he’s 70, on clopidogrel, and takes pantoprazole. He never knew why. I showed him this. He said, ‘So I’m not just taking pills because the doctor said so?’ I told him yes, but now he knows why. Small wins.
Wendy Stanford
6 November 2025There’s a deeper question here, isn’t there? We’ve turned medicine into a series of algorithmic checkboxes - risk factors, scores, guidelines - but we’ve lost the human element. Who is this person? What are they afraid of? What does their body actually need? We’re treating risk profiles, not people. And in that reduction, we create more anxiety, not less. The PPI isn’t the problem. The system is.
Jessica Glass
6 November 2025Of course you don’t need a PPI if you’re ‘young and healthy.’ You’re probably one of those people who thinks kale fixes everything. Meanwhile, my 74-year-old mom had a bleed last year. She’s on pantoprazole. And she’s alive. So maybe stop preaching to the choir and help the people who actually need it.
Krishna Kranthi
8 November 2025bro just ask your doc if you need it. if they say yes, take it. if they say no, don’t. stop overthinking. i take pantoprazole with ticagrelor. no issues. my uncle took omeprazole with clopidogrel. he’s fine. maybe its all just noise?
Lilly Dillon
8 November 2025I’ve been on PPIs for 8 years. I stopped last year after reading this. No stomach pain. No bleeding. Just… quiet. Sometimes the best medicine is not taking anything at all.
Peter Feldges
9 November 2025Your point about real-world adherence is well-taken, but the meta-analysis you referenced still showed a 15% relative risk increase in cardiovascular events with omeprazole + clopidogrel in patients with poor metabolizer genotypes - a group that’s not rare. Genetic testing isn’t perfect, but it’s becoming more accessible. Until it’s universal, we err on the side of caution. And that’s why guidelines recommend alternatives.