Obstructive sleep apnea isn’t just loud snoring. It’s when your throat muscles relax so much during sleep that your airway closes off-sometimes dozens of times an hour-cutting off oxygen and jolting you awake without even realizing it. You might feel tired all day, struggle to focus, or wake up with a dry mouth and headache. Left untreated, it raises your risk for high blood pressure, heart attacks, and strokes. The good news? There are effective ways to treat it. The most common is CPAP therapy, but it’s not the only option-and for some people, it’s not the best one.
How CPAP Therapy Works
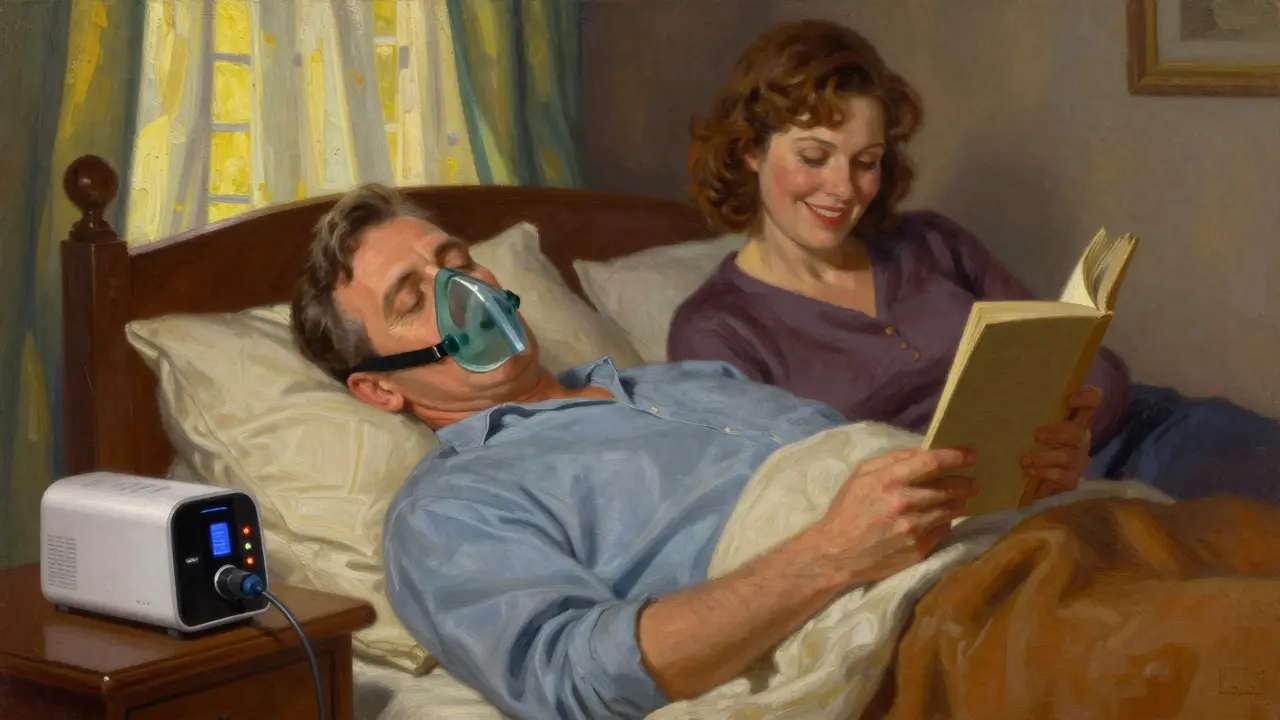
CPAP stands for Continuous Positive Airway Pressure. It’s a machine that gently blows air through a mask you wear while sleeping. That air pressure keeps your throat open so you can breathe normally. It’s not a cure, but it stops the apneas from happening. The first CPAP device was developed in 1981, and since then, it’s become the gold standard for treating moderate to severe obstructive sleep apnea.
Modern CPAP machines are quiet, lightweight, and smart. They track your usage, detect leaks, and adjust pressure automatically. Most people use a nasal mask, full-face mask, or nasal pillows. The pressure settings usually range from 4 to 20 cm H₂O, depending on how severe your apnea is. A sleep study determines the right pressure for you.
When used correctly-for at least 7 hours a night-CPAP can cut your apnea-hypopnea index (AHI) from 39 events per hour down to under 7. That means fewer awakenings, deeper sleep, and better oxygen levels. Studies show it also lowers blood pressure by 5-10 mmHg and improves daytime alertness by up to 40%.
Why Many People Struggle With CPAP
Even though CPAP works, it doesn’t work for everyone. About half of people prescribed CPAP stop using it within the first year. The reasons are simple: discomfort, inconvenience, and frustration.
Mask leaks are the #1 complaint. If the seal isn’t perfect, air escapes, and the pressure drops. That leads to dry mouth, nasal congestion, or even stomach bloating. About 62% of people who start with a nasal mask switch to a full-face mask within six months because they breathe through their mouth.
Then there’s the claustrophobia. Some people feel trapped under the mask. Others hate the noise-even though modern machines are as quiet as a whisper (26-30 decibels). Traveling with a CPAP is a hassle. And cleaning the mask, tubing, and humidifier every week? It feels like another job.
One user on Reddit wrote: "I’ve tried five masks over two years. Still can’t wear it more than two hours. The feeling of being suffocated is unbearable." That’s not rare. In fact, 12% of users report claustrophobia as a dealbreaker.
CPAP Adherence: The Real Problem
Here’s the harsh truth: CPAP only works if you use it. And most people don’t use it enough.
Insurance companies require you to use your CPAP for at least 4 hours a night, 70% of the time, to keep coverage. About 70% of users hit that mark. But that still means 30% don’t. And even among those who do, many are only using it for 4-5 hours-not the 7+ hours needed to fully reverse the damage.
A 2020 study showed that if you use CPAP for only 2 hours a night, your apnea is still moderate to severe. At 4 hours, it’s still mild. You need 8 hours to get back to normal. That’s why some doctors say CPAP’s biggest weakness isn’t the machine-it’s human behavior.
That’s where alternatives come in.

Oral Appliances: A Simpler Option
Oral appliances-custom-fitted mouthpieces-are the most common alternative to CPAP. They look like sports mouthguards or orthodontic retainers. They work by gently moving your lower jaw forward, which pulls your tongue and soft tissues away from the back of your throat.
They’re not as powerful as CPAP for severe apnea, but they’re much easier to live with. A 2017 review from the American Academy of Dental Sleep Medicine found that people use oral appliances 77% of nights after a year. CPAP? Only 4-5 hours a night on average.
People prefer them because they’re quiet, portable, and don’t feel invasive. One user on Amazon wrote: "I travel for work all the time. I used to hate dragging my CPAP. Now I just toss this in my pocket. I sleep better, and my wife says I stopped snoring."
They’re FDA-cleared for mild to moderate OSA, and some doctors prescribe them for severe cases too-especially if CPAP failed. The downside? They can cause jaw pain, tooth movement, or bite changes over time. That’s why you need a dentist who specializes in sleep apnea to fit them.
Surgery and Implants: When Less Is More
Surgery sounds like a permanent fix, but it’s rarely that simple. Uvulopalatopharyngoplasty (UPPP)-removing excess tissue from the throat-has a success rate of only 40-60%. Many people still need CPAP afterward.
A newer option is hypoglossal nerve stimulation, known as Inspire therapy. It’s a small implant in your chest that stimulates the nerve controlling your tongue. When you sleep, it gently moves your tongue forward to keep your airway open. Clinical trials show it reduces apnea events by 79%.
But it’s invasive. It requires surgery, recovery time, and costs around $35,000 out-of-pocket. Insurance covers it only for people who can’t use CPAP and have moderate to severe OSA. It’s not for everyone-but for those who qualify, it’s life-changing.
Other Alternatives: Positional Therapy and Lifestyle
Not everyone has apnea all night. Some people only have it when they sleep on their back. That’s called positional OSA. For them, a simple device like NightBalance can help. It’s a soft belt that vibrates gently when you roll onto your back, nudging you to your side. One study showed it cuts apnea events by 51%.
Lifestyle changes matter too. Losing 10% of your body weight can reduce apnea severity by half. Quitting alcohol and sedatives helps-both relax your throat muscles. Sleeping on your side, elevating your head, and treating nasal allergies can also make a difference.
These aren’t cures, but they’re low-risk ways to improve symptoms-even if you’re still using CPAP or an oral appliance.

Choosing the Right Treatment for You
There’s no one-size-fits-all solution. Your best option depends on your apnea severity, anatomy, lifestyle, and tolerance.
- Severe OSA (AHI ≥ 30): CPAP is still the top choice. If you can’t tolerate it, Inspire therapy may be an option.
- Moderate OSA (AHI 15-29): CPAP or oral appliance-choose based on comfort and adherence. Many people do better with an oral device.
- Mild OSA (AHI 5-14): Try lifestyle changes first. If symptoms persist, an oral appliance is often more effective than CPAP.
Also consider your personality. If you’re someone who values simplicity and hates gadgets, an oral appliance might suit you better. If you’re tech-savvy and don’t mind routines, CPAP with auto-adjusting pressure and a humidifier could be ideal.
And don’t ignore the emotional side. If you feel anxious or claustrophobic around masks, talk to your doctor. There are smaller masks, softer materials, and desensitization techniques that help.
What’s Next for Sleep Apnea Treatment
The field is changing fast. New CPAP machines now detect breathing problems before they become full apneas. Apps like Nightware use biofeedback to help users fall asleep faster and stay asleep longer-boosting CPAP adherence by 22% in early trials.
Researchers are also exploring personalized pressure settings based on 3D scans of your airway. Imagine a machine that learns your unique breathing pattern and adjusts in real time-not just based on events, but on your body’s signals.
One big shift coming: doctors are starting to test your arousal threshold. That’s how easily you wake up during sleep. People with a high threshold wake up easily and get big cognitive benefits from CPAP. People with a low threshold barely notice the interruptions-and get little benefit. For them, an oral appliance or weight loss might be a smarter first step.
The goal isn’t just to treat apnea. It’s to treat you.
Getting Started: What to Do Now
If you suspect you have obstructive sleep apnea, don’t wait. Start with a home sleep test or an overnight study at a sleep center. That’s the only way to know your AHI and severity.
Once you have a diagnosis:
- Ask your doctor about all treatment options-not just CPAP.
- Try CPAP with a sleep specialist who offers follow-up visits. Don’t give up after a week.
- If CPAP doesn’t work, ask for a referral to a dental sleep specialist for an oral appliance.
- Consider weight loss, positional therapy, or nasal strips if your apnea is mild.
- Track your progress. Use your CPAP app or journal how you feel in the morning.
Treatment isn’t a one-time decision. It’s a process. What works today might not work next year. Be open to change. Your sleep-and your health-depend on it.
Is CPAP the only treatment for sleep apnea?
No, CPAP is the most common and effective treatment for moderate to severe obstructive sleep apnea, but it’s not the only one. Oral appliances, positional therapy, weight loss, and surgical options like hypoglossal nerve stimulation are proven alternatives. The best choice depends on your severity, anatomy, and ability to stick with the treatment.
Can I use an oral appliance instead of CPAP?
Yes-if you have mild to moderate obstructive sleep apnea, an oral appliance is often just as effective as CPAP and much easier to use long-term. For severe cases, CPAP is usually recommended first, but some patients with severe apnea who can’t tolerate CPAP do well with an oral device. A dentist trained in sleep medicine can fit you properly.
Why do so many people stop using CPAP?
The most common reasons are mask discomfort, nasal dryness, claustrophobia, and difficulty traveling with the machine. Many users struggle with leaks or feel the air pressure is too strong. About half of people stop using CPAP within the first year. But most of these issues can be solved with the right mask, humidifier, or adjustment-don’t give up without trying different options.
Does losing weight help with sleep apnea?
Yes. Losing just 10% of your body weight can reduce the number of apnea events by half. Excess weight, especially around the neck, puts pressure on your airway. Weight loss alone can eliminate mild sleep apnea and make other treatments like CPAP or oral appliances work better.
How do I know if my CPAP is working?
Check your machine’s data. Most modern CPAPs track how many hours you use it each night, your residual apnea-hypopnea index (AHI), and leak rates. If your AHI drops below 5 and you’re using it 7+ hours a night, it’s working. You should also feel more alert during the day, sleep better at night, and have less snoring. If not, talk to your doctor-your pressure might need adjusting.
Is sleep apnea treatment covered by insurance?
Yes, most insurance plans-including Medicare-cover CPAP machines, oral appliances, and sleep studies if you have a diagnosis of obstructive sleep apnea. CPAP machines usually require a prescription and proof of usage (4+ hours per night, 70% of nights). Oral appliances often require a referral to a dental sleep specialist. Always check with your provider before starting treatment.
If you’ve been told you have sleep apnea and you’re not sleeping well, it’s not your fault. The system isn’t perfect. But better tools, smarter approaches, and more options exist than ever before. The key is finding what fits your life-not forcing yourself to fit the treatment.






Matt Davies
19 December 2025CPAP is like a digital pacifier for your airway-works wonders if you don’t fight it. I used to hate mine, but after switching to nasal pillows and adding a humidifier? Night and day. My wife says I snore like a toddler now. 😴❤️
Isabel Rábago
21 December 2025People act like CPAP is some kind of punishment, but if you’re too lazy to lose weight or change your sleep position, then yeah, you’re gonna need the machine. It’s not the device’s fault you won’t adapt. This isn’t a trend-it’s a medical necessity.
Mike Rengifo
21 December 2025I tried CPAP for three weeks. Mask felt like a sci-fi helmet. Then I got an oral appliance. Quiet. No cords. Fits in my pocket. Wife says I’m less of a chainsaw at night. I call it my sleep superhero. No drama, just results.
Dev Sawner
23 December 2025The statistical non-adherence rates to CPAP therapy are alarming and indicative of a systemic failure in patient education and behavioral reinforcement. One cannot simply prescribe a device and expect compliance without addressing the psychosocial determinants of adherence. The data is unequivocal.
Moses Odumbe
24 December 2025Bro, CPAP is NOT the only way. I went from 42 AHI to 8 with a custom mouthguard and lost 15 lbs. No machine. No wires. Just me, my pillow, and sweet, sweet uninterrupted sleep. 🙌 Also, if you’re still using a full-face mask in 2024… maybe try not breathing through your mouth? 🤔
bhushan telavane
24 December 2025In India, many still think snoring is normal. My uncle had severe apnea for 12 years, thought it was just "old age." Got diagnosed after collapsing at a wedding. Now he uses CPAP. Life changed. But access? Still a nightmare outside cities. Need more awareness.
Mahammad Muradov
26 December 2025The claim that oral appliances are effective for severe OSA is misleading. The AASM guidelines are clear: CPAP remains first-line for AHI > 30. Any deviation without documented failure of CPAP constitutes substandard care. Do not confuse anecdotal success with clinical evidence.
mark shortus
27 December 2025I WAS A CPAP HATER. I THOUGHT IT WAS A PRISON. I HATED THE NOISE. I HATED THE MASK. I HATED THE TUBING. I HATED THE HUMIDIFIER. I HATED THE CLEANING. I HATED THE TRAVEL. I HATED THE FEELING OF BEING TIED DOWN. THEN I GOT A NEW MASK. AND A NEW MINDSET. AND NOW I’M A CPAP FANATIC. I SLEEP LIKE A BABY. I’M ALIVE AGAIN. DON’T GIVE UP. 🙏😭
Emily P
28 December 2025I’m curious-how do people decide between Inspire and an oral appliance? Is it mostly based on cost, or are there other factors like jaw structure or tongue size that make one better than the other?
Vicki Belcher
28 December 2025To anyone struggling with CPAP: you’re not broken. You just haven’t found your fit yet. I tried 7 masks, 3 machines, and a sleep coach. Took 11 months. Now I sleep 8 hours. No alarms. No guilt. Just peace. 💙 Don’t quit. Your future self will thank you.