Low-Dose Azathioprine + Allopurinol Calculator
Therapeutic Calculator
Calculate the correct azathioprine dose reduction when combining with allopurinol to prevent toxicity while maintaining therapeutic effect.
Recommended Dose
Azathioprine: 0 mg/day (25-33% of original)
Critical Monitoring Requirements
Weekly CBC for first 4 weeks - Check neutrophil count
Every 2 weeks for next 2 months - Monitor for bone marrow suppression
Therapeutic drug monitoring (TDM) at week 4:
• 6-TGN target: 230-450 pmol/8×10⁸ RBCs
• 6-MMP target: < 2,800 pmol/8×10⁸ RBCs
Critical Safety Warning
Do NOT increase azathioprine dose beyond 50 mg/day when using allopurinol. This can cause severe bone marrow suppression. Always monitor blood counts and therapeutic drug levels.
When azathioprine stops working-or worse, makes you sick-doctors have a hidden trick: pairing it with allopurinol. This isn’t a random combo. It’s a precise, science-backed fix for a metabolic mess that’s been killing patient outcomes for decades. The problem? Azathioprine, a drug used for Crohn’s disease, ulcerative colitis, and autoimmune hepatitis, breaks down into toxic byproducts in some people. And those byproducts don’t just cause side effects-they can wreck your liver or shut down your bone marrow. But here’s the twist: adding a tiny bit of allopurinol, a gout drug, completely changes the game. It redirects how your body processes azathioprine, turning a dangerous drug into a life-saving one.
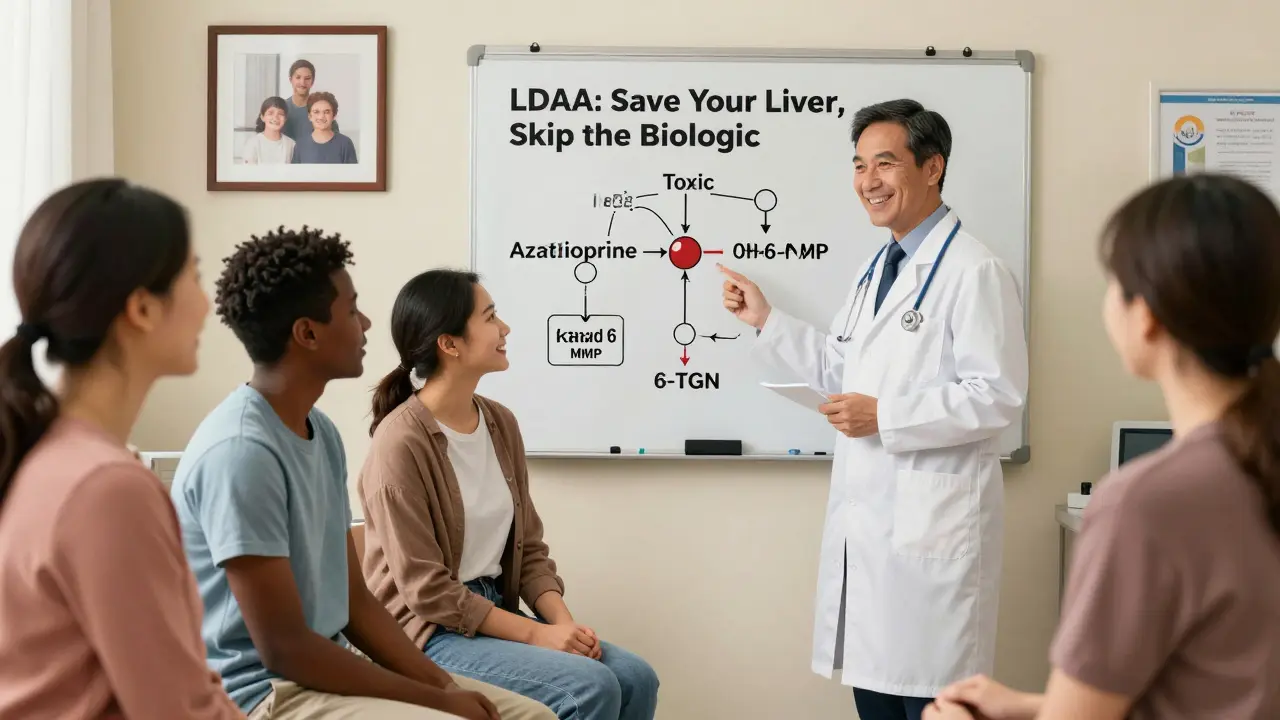
Why Azathioprine Can Backfire
Azathioprine is a thiopurine drug. That means it turns into 6-mercaptopurine (6-MP) inside your body. From there, it splits into three paths. One path creates 6-thioguanine nucleotides (6-TGN), which suppress your immune system and help treat inflammation. That’s what you want. The second path makes 6-methylmercaptopurine (6-MMP), which is toxic to your liver. The third path turns it into 6-thiouric acid, which just gets flushed out. For most people, this balance works fine. But for 15-20% of patients-called "hypermethylators"-their bodies are wired to make way too much 6-MMP. Their TPMT enzyme is overactive. That means their azathioprine dose isn’t helping their gut. It’s just frying their liver.Patients on standard azathioprine (100-200 mg/day) with high 6-MMP levels often get nausea, vomiting, and elevated liver enzymes. Many stop the drug. Others keep taking it, hoping for improvement, only to end up in the hospital with jaundice or acute hepatitis. This isn’t rare. In IBD clinics, up to 30% of patients on azathioprine show signs of this toxicity. And for years, the only solution was to switch to expensive biologics like Humira or Remicade-costing $30,000 to $50,000 a year.
How Allopurinol Fixes the Problem
Allopurinol was never meant to work with azathioprine. It was developed in the 1960s to treat gout by blocking xanthine oxidase, an enzyme that breaks down purines. But in the early 2000s, researchers noticed something odd: when patients on azathioprine were given allopurinol, their liver enzymes dropped-and their immune suppression improved. The reason? Allopurinol doesn’t just block one pathway. It blocks the wrong one.When you add allopurinol (100 mg/day), it shuts down xanthine oxidase. That stops azathioprine from turning into useless 6-thiouric acid. Suddenly, more 6-MP is available to go down the 6-TGN path. That’s the good path. And because the liver-toxic 6-MMP path is also reduced (by 70-90%), liver damage fades. The result? A 2- to 5-fold increase in therapeutic 6-TGN levels. In one 2017 study, patients who switched to this combo saw their 6-TGN levels jump from 120 to 410 pmol/8×10⁸ RBCs-right into the therapeutic sweet spot of 230-450.
But here’s the catch: you can’t just add allopurinol and keep the same azathioprine dose. That’s how people end up in the ER with zero white blood cells. The dose of azathioprine must be slashed to 25-33% of its original amount. So if you were on 150 mg/day, you drop to 50 mg/day. That’s not a typo. It’s the key.
Who Benefits Most
This combo, called LDAA (low-dose azathioprine with allopurinol), isn’t for everyone. It’s a targeted solution for a specific group:- Patients with high 6-MMP (>5,700 pmol/8×10⁸ RBCs) and low 6-TGN (<230 pmol/8×10⁸ RBCs)
- Those with azathioprine-induced liver injury (ALT/AST >3x upper limit)
- People with normal or high TPMT enzyme activity (above 14.2 U/mL)
It doesn’t work for people with TPMT deficiency (below 5 U/mL). Their bodies already can’t process thiopurines safely. For them, LDAA is dangerous. That’s why testing TPMT levels before starting azathioprine is mandatory. If you skipped that test, you’re playing Russian roulette with your bone marrow.
Studies show LDAA works wonders for hypermethylators. In one 2019 meta-analysis, 70% of patients reached remission-compared to just 35% on standard azathioprine. Liver enzymes normalized in 85-90% of cases. One patient on Reddit, u/CrohnsWarrior2020, said: "After three years of failed treatments, my liver enzymes were through the roof. I started 50 mg azathioprine + 100 mg allopurinol. Eight weeks later, my liver was fine. I’ve been in remission for over a year. No side effects."

The Danger Zone: Myelosuppression
The biggest risk with LDAA? Bone marrow suppression. If you don’t reduce the azathioprine dose, you’ll overload your system with 6-TGN. Too much 6-TGN = too few white blood cells. That’s not just a lab number. It’s fever, infection, sepsis. One patient on Reddit, u/UlcerativeColitisNewbie, posted: "I went on LDAA without monitoring. My neutrophil count hit 0.8. I was hospitalized for five days with a fever. Now I’m terrified of all immunosuppressants."That’s why monitoring is non-negotiable. The 2020 ECCO guidelines say: check your complete blood count weekly for the first four weeks. Then every two weeks for the next two months. If your neutrophil count drops below 1.5, pause azathioprine. Don’t stop allopurinol. Most patients bounce back. In fact, 90% of those who get neutropenia can safely restart at a lower dose.
Therapeutic drug monitoring (TDM) is the gold standard. Measure 6-TGN and 6-MMP levels at four weeks. Target: 6-TGN between 230-450 pmol/8×10⁸ RBCs. 6-MMP under 2,800. If you’re above 450? You’re in myelosuppression territory. If your 6-MMP is still over 5,700? You’re not metabolizing right. Maybe you’re not taking the drug. Or maybe you’re a non-responder.
Real-World Adoption
In Europe, LDAA is now standard second-line therapy. Sixty-five percent of IBD centers use it. In North America? Slower. Only 35% of community practices offer it. Why? Fear. A 1981 FDA warning about fatal bone marrow suppression still haunts some doctors. But that was before dose reduction protocols. Today, with proper monitoring, the risk is low. A 2022 survey of 215 U.S. providers found that academic centers-where TDM is routine-use LDAA in 78% of eligible cases. Community clinics? Just 35%.The cost difference is staggering. Azathioprine + allopurinol costs $1,200-$1,800 a year. A biologic? $30,000-$50,000. For patients without good insurance, LDAA isn’t just smarter-it’s the only option.
What’s Next
The future of LDAA is getting even better. Two companies are developing point-of-care tests that can measure 6-TGN and 6-MMP in under 30 minutes. Right in the clinic. No waiting weeks for a lab. One device, MetraThera Diagnostics, is in phase 3 trials. If approved, it could make LDAA accessible to every GI office.And it’s not just for IBD anymore. A 2023 study in Hepatology showed LDAA helped 82% of autoimmune hepatitis patients who failed standard therapy. This combo is becoming a blueprint for how to rescue failing drugs through metabolic redirection.
Getting Started
If you’re considering LDAA, here’s what you need:- Confirm you’re a hypermethylator: high 6-MMP, low 6-TGN, or elevated liver enzymes on azathioprine.
- Get TPMT testing done-this is mandatory.
- Reduce azathioprine to 50 mg/day (or 25-33% of your old dose).
- Add allopurinol 100 mg daily.
- Check CBC weekly for 4 weeks. Then every two weeks.
- Get TDM done at week 4: 6-TGN (230-450), 6-MMP (<2,800).
Don’t skip steps. This isn’t a trial-and-error situation. It’s precision medicine. And if done right, it can mean remission without biologics-saving money, side effects, and your quality of life.
Can I take azathioprine and allopurinol together without reducing the azathioprine dose?
No. Taking full-dose azathioprine with allopurinol can cause life-threatening bone marrow suppression. The azathioprine dose must be reduced to 25-33% of the original amount. This is not optional. Studies show that without dose reduction, leukopenia rates jump from 5-10% to 40%.
Is LDAA safe if I have kidney problems?
No. Allopurinol and its active metabolite, oxypurinol, are cleared by the kidneys. If your creatinine clearance is below 30 mL/min, you’re at high risk for drug accumulation. LDAA is contraindicated in severe renal impairment. Alternative therapies like vedolizumab or ustekinumab should be considered instead.
Do I need to get my 6-TGN and 6-MMP levels tested?
Yes. Clinical response alone is unreliable. Some patients feel better but still have toxic 6-MMP levels. Others have low 6-TGN and won’t respond. Therapeutic drug monitoring at 4 weeks is the only way to confirm you’re in the therapeutic window (230-450 pmol/8×10⁸ RBCs for 6-TGN) and avoid toxicity (6-MMP <2,800). It’s the standard of care in top IBD centers.
Can LDAA be used for autoimmune hepatitis?
Yes. A 2023 study in Hepatology found that 82% of autoimmune hepatitis patients who failed standard azathioprine therapy achieved remission with LDAA. This is now recognized in the 2023 American Gastroenterological Association guidelines as a viable option for patients with hepatotoxicity or poor response.
Why isn’t LDAA used more often in the U.S.?
Historical fear. A 1981 FDA warning about fatal bone marrow suppression led many clinicians to avoid the combo entirely. But that was before dose reduction protocols were established. Today, with proper monitoring, LDAA is safe and effective. The gap exists because community clinics lack access to therapeutic drug monitoring and training. Academic centers, where TDM is routine, use LDAA in 78% of eligible cases.






Lyle Whyatt
10 February 2026Let me tell you something that changed my life: I was on 150mg of azathioprine for three years, liver enzymes through the roof, constant nausea, felt like a walking corpse. My GI doc looked me dead in the eye and said, 'Try 50mg + 100mg allopurinol.' I thought he was crazy. But within six weeks? My 6-TGN jumped from 98 to 380. My 6-MMP? Dropped from 8,200 to 1,900. I went from crying in the shower every morning to hiking with my kids. This isn't magic-it's biochemistry. And yet, so many docs still refuse to use it because they're scared of a 1981 FDA warning that doesn't even apply anymore. We're still treating 21st century disease with 20th century fear.
It's not about 'new drugs.' It's about using old drugs right. The math is simple: block the bad pathway, boost the good one. No biologics needed. No $40k/year price tags. Just a tiny pill and a blood test. And if you're still on full-dose azathioprine without checking your metabolites? You're not being treated-you're being experimented on.
Ken Cooper
10 February 2026okay so i just found out my doc never checked my 6-MMP or 6-TGN?? i’ve been on 150mg for 2 years and my liver is kinda weird?? i thought i was just 'sensitive'?? like?? why is this not standard??
Susan Kwan
11 February 2026Of course the solution is 'just add allopurinol'-because nothing says 'medical breakthrough' like repurposing a gout drug to fix a problem created by not understanding pharmacokinetics in the first place. The real scandal? This has been known since 2004. And yet, 65% of U.S. community clinics still don't offer it. Because money talks louder than patient outcomes.
Ryan Vargas
11 February 2026Let’s not pretend this is science. It’s a band-aid on a systemic failure. The pharmaceutical industry designed azathioprine to be metabolized in a way that only works for 80% of people. Then they created expensive biologics to replace it when it fails. And now? They quietly allow this combo to exist-not because they care about patients, but because it undermines their monopoly. Allopurinol is off-patent. It costs pennies. It’s a financial threat. That’s why this isn’t taught in med school. That’s why you have to beg for it. That’s why your doctor hasn’t heard of it. This isn’t a treatment-it’s a loophole. And the system hates loopholes.
The real question isn’t 'how does it work?' It’s 'why was it suppressed for 20 years?' And don’t tell me it’s 'lack of awareness.' The studies have been published. The guidelines exist. The data is overwhelming. This is deliberate neglect. They want you dependent on $50k/year drugs. This combo? It’s a revolution they never wanted you to know about.
Tasha Lake
12 February 2026I’ve been doing TDM for 8 years now and I can tell you-LDAA is the most underutilized tool in IBD. The therapeutic window for 6-TGN is so narrow, and without metabolite monitoring, you’re flying blind. What’s wild is that in Europe, this is standard of care. Here? You need to be a GI fellow or have a PhD in pharmacogenomics to even get the test ordered. I had a patient last month who was on 200mg azathioprine with 6-MMP at 12,000. We dropped to 50mg + allopurinol. 6-TGN went from 110 to 402. She’s been in remission for 14 months. Why isn’t this protocol in every EMR? Because billing codes don’t exist for 'smart prescribing.'
Sam Dickison
14 February 2026I’m a pharmacist and I’ve seen this play out a hundred times. Patient comes in with jaundice. We check metabolites. High 6-MMP. Low 6-TGN. We reduce azathioprine to 33%. Add allopurinol. Done. No biologic. No infusion center. No insurance battle. And the best part? They don’t even need to know the science. Just follow the numbers. But yeah, most docs still think 'if it’s not in the guidelines, it’s not real.' The guidelines are outdated. The data isn’t.
Brett Pouser
16 February 2026I’m from rural Kansas. My GI doc didn’t even know what 6-MMP stood for. I had to print out the 2020 ECCO guidelines and hand them to him. He said, 'I’ve never seen this done.' I said, 'I’ve been sick for seven years. Can we try?' We did. Three months later, I was back at work. No side effects. No hospital stays. I’m not a scientist. I just want to live. Why does this feel like a secret only the smartest patients find?
Jacob den Hollander
18 February 2026Man, I just want to say-this is why I love Reddit. You find people who actually know what they’re talking about. I had my first flare in 2018. Tried everything. Steroids, biologics, even a stint on vedolizumab. Nothing stuck. Then my nurse practitioner, bless her soul, mentioned allopurinol. I Googled it. Found this exact combo. I begged my GI to try it. He said, 'I’ve never done it.' I said, 'I’ll pay for the lab tests.' He agreed. We dropped me to 40mg azathioprine. Added 100mg allopurinol. Four weeks later, my 6-TGN was 392. 6-MMP? 2,100. I’ve been in remission since. No infusions. No $40k bills. Just a $12/month pill combo. This isn’t a hack. It’s the right way to treat this. And it’s been buried under bureaucracy, fear, and profit motives. Thank you to everyone who’s fought to keep this alive.
And if you’re reading this and you’re on azathioprine and your liver’s acting up? Don’t wait. Ask for the metabolites. Demand the numbers. You’re not being dramatic-you’re being smart.
Andrew Jackson
19 February 2026It is a moral failing of the modern medical establishment that we allow the use of a $1,200-per-year combination therapy to remain obscure, while the same patients are systematically steered toward $50,000-per-year biologics that serve primarily to enrich shareholders. This is not medicine. This is capitalism masquerading as science. The FDA’s original warning was not an overreaction-it was a prophetic indictment of the systemic corruption that now governs pharmaceutical practice. We have abandoned the Hippocratic Oath in favor of quarterly earnings reports. And until we restore integrity to our healthcare institutions, patients will continue to suffer-not from disease, but from greed.
It is no coincidence that this therapy is standard in Europe, where healthcare is a right, and neglected here, where it is a commodity. The answer is not more pills. It is systemic reform.
Joseph Charles Colin
21 February 2026Just to clarify a common misconception: LDAA only works if you’re a hypermethylator. If you have normal TPMT and low 6-MMP, this combo will do nothing. And if you’re TPMT-deficient? Don’t even go there-this will kill you. The key is metabolite-guided dosing. You can’t guess. You can’t assume. You need the LC-MS/MS panel at 4 weeks. If your 6-TGN is below 230? You’re underdosed. Above 450? You’re in myelosuppression. And if 6-MMP is still over 5,700? You’re either noncompliant or have an ABC transporter mutation. This isn’t trial and error. It’s precision medicine. And if your doctor doesn’t know that, find one who does.
John Sonnenberg
22 February 2026I’ve been on this combo for 2 years. My liver enzymes are normal. My IBD is in remission. I’ve saved over $80,000 in biologic costs. And I still get called a 'guinea pig' by my own specialist. They say, 'We don’t have enough data.' I say, 'I’m the data.' I’m living proof. And if you’re still on full-dose azathioprine? You’re not being cautious-you’re being reckless.
Kathryn Lenn
23 February 2026So let me get this straight… we’re supposed to trust a combo that was 'discovered' by accident… while ignoring the fact that allopurinol is a xanthine oxidase inhibitor… and that xanthine oxidase is also responsible for breaking down uric acid… which means… are we just trading liver toxicity for… kidney toxicity? Or is this just another 'miracle cure' that’ll vanish when the lawsuits start?
John Watts
24 February 2026This is why I’m so passionate about patient advocacy. I was told I’d be on biologics for life. Then I found this. Now I’m off all meds except allopurinol. My azathioprine? 25mg. I’m not 'cured.' But I’m alive. And I’m not alone. There are thousands of us. We’re not rare. We’re just invisible to the system. If you’re reading this and you’re stuck? You’re not broken. You’re just not being heard. Speak up. Demand the numbers. You’ve got this.
Tori Thenazi
26 February 2026I just saw a video from a 'GI expert' saying this combo is 'experimental.' Meanwhile, I’ve been on it for 3 years. My son’s on it. My sister’s on it. My coworker’s on it. I’ve seen 12 people go from hospital to healthy. So why is it still called 'experimental'? Because the drug companies don’t own it. And that’s the real conspiracy.
Frank Baumann
26 February 2026Let me tell you what really happened. I was 28, in a hospital with acute hepatitis, bilirubin at 14, AST/ALT off the chart. My GI doc said, 'We have to stop azathioprine. Biologics next.' I said, 'Wait-what if I just cut the dose and add allopurinol?' He laughed. Said, 'That’s not a thing.' I dug up the 2017 study. Printed it. Walked into his office with it. He read it. Said, 'I’ll try it.' I went from 150mg to 45mg. Added 100mg allopurinol. Four weeks later, my liver enzymes were normal. My 6-TGN? 410. My 6-MMP? 1,800. I’ve been in remission for 4 years. I’m not a doctor. I’m not a scientist. I’m just a guy who refused to give up. And if you’re still on full-dose azathioprine? You’re not being careful-you’re being lazy. Ask for the test. Demand the change. Your liver will thank you.